Peripheral Quantitative Computed Tomography (pQCT, HR-pQCT)
Peripheral QCT is another non-invasive, relatively safe imaging modality that can be used to diagnose osteoporosis. Whereas DXA measures areal BMD, pQCT measures volumetric BMD (vBMD), which is defined as bone mineral content (BMC) per unit volume in g/cm3. vBMD stands alongside aBMD as a surrogate outcome for fracture risk reduction. In addition to assessing volumetric bone density, pQCT can also differentiate cortical bone from trabecular bone and quantify architecture. However, pQCT is available as a clinical diagnostic tool in only a few countries.
High-resolution pQCT (HR-pQCT) improves upon the resolution of standard pQCT imaging and is now available with as fine as 42µm resolution. This imaging modality gives detailed information on the microarchitecture of peripheral bone but is not widely available outside of research applications in North America and is not recommended for cross-sectional studies at this time.
The current official positions of the International Society for Clinical Densitometry (ISCD) (Engelke et al. 2008, Kanis et al. 2015, Adams et al. 2014, Zysset et al. 2015), does not yet recommend routine use of pQCT for diagnosis of osteoporosis, fracture risk prediction or monitoring treatment effectiveness. This position is in part due to the incompatibility of pQCT data with DXA derived T-scores, inconsistency in measurement sites and bone analysis, lack of normative studies, and specific treatment thresholds (Engelke et al. 2008, Adams et al. 2014, Zysset et al. 2015). An example of a pQCT image can be seen in Figure 3.
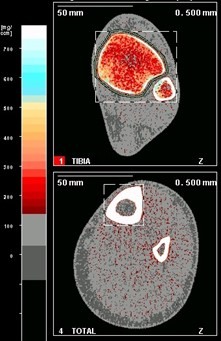 Figure 3. Example of pQCT data. Upper panel represents the tibial epiphysis (predominantly trabecular bone; red colour tones). Lower panel represents the tibial diaphysis (predominantly cortical bone; white colour tones).
Figure 3. Example of pQCT data. Upper panel represents the tibial epiphysis (predominantly trabecular bone; red colour tones). Lower panel represents the tibial diaphysis (predominantly cortical bone; white colour tones).