Primary Care and Skin Health

Stage 1 Pressure Ulcer
Pressure Ulcers (PUs) are among the most common complications and highest causes of re-hospitalization for people with SCI. They can even be life-threatening if infections develop and spread to the blood, bone, or heart.
PUs most often occur due to lying or sitting in one position for too long, improper padding or cushioning, and/or clothes/shoes fitting too tightly.
If extended treatment or prolonged bed rest is necessary, your patient is even more at risk for additional PUs and missing school, work, and other important life activities.
—
Risk factors for Pressure Ulcers include:
- Higher level of injury/Lower Mobility (more parts of skin touching surfaces for longer periods)
- Bowel/bladder incontinence (excess moisture on skin increases risks for PUs)
- Darker skin color (harder to see early stages of PUs)
- Lower income/lower social support (less like to get early assessment/treatment)
A complete approach to avoiding damage to the skin is necessary.
The majority of research and recommendations on skin issues for people with SCI are to do with PUs…BUT lack of sensation (i.e., the body’s warning signal) makes people with SCI vulnerable to burns, frostbite, and bumps/bruises/cuts/scratches that do not heal.
Most pressure sores are preventable! Making sure that you and your patients are educated about preventing pressure sores and other skin injuries is the best way to keep them healthy and out of hospital.
- Screen for and minimize known risk factors for Pressure Ulcers in your patients, like previous history of PUs, smoking, and other health issues like diabetes, high blood pressure, high cholesterol, poor nutrition, and being over/under weight.
- Ask about all surfaces they are in contact with – e.g., wheelchair cushions, beds, chairs, transfer boards, toilet seat
- Assess any need for additional health care/home care support – Seating specialist, OT, PT, wound nurse, social worker, physiatrist, home healthcare aide/nurse may all need to be part of your patient’s health care team
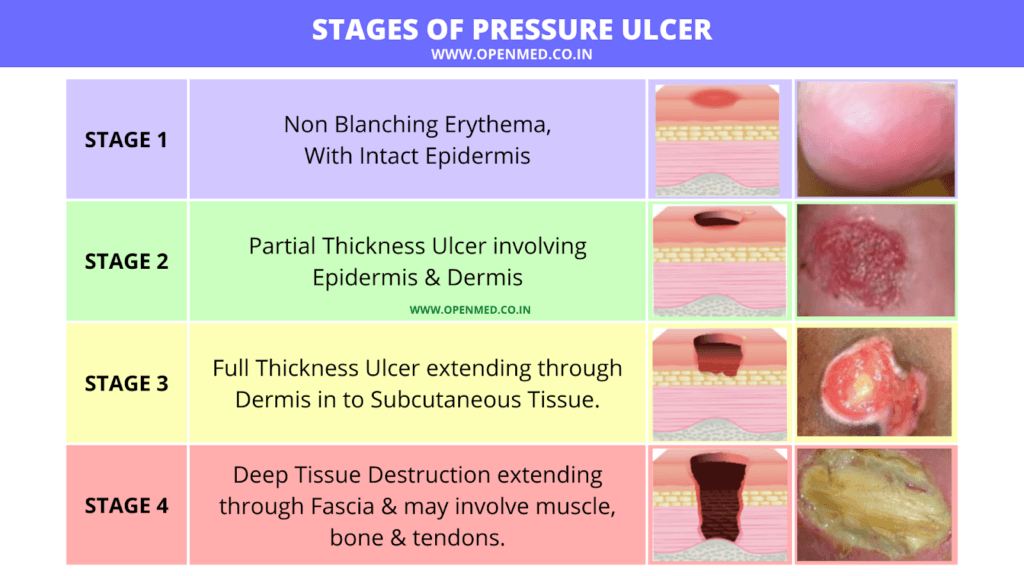
Stages of Pressure Ulcers. https://www.openmed.co.in/2022/08/stages-of-pressure-ulcer.html. CC BY-NC-SA 4.0
If you do discover a Pressure Ulcer, the most important things you need to know are:
- Where is it?
- Why did it start?
- Why isn’t it healing?
Take note of wound location, size, appearance of wound bed.
Consult with relevant members of healthcare team – e.g., wound care, home health aide, wheelchair specialist – in order to develop a full treatment plan.
Generally speaking, Stage I or II PUs can be treated either in Primary Care or with standard wound care nursing. Stage III or IV wounds will require specialist and/or surgical intervention.
It is recommended that a full skin exam is performed at the initial appointment (to establish a baseline) and that skin is asked about at every appointment.
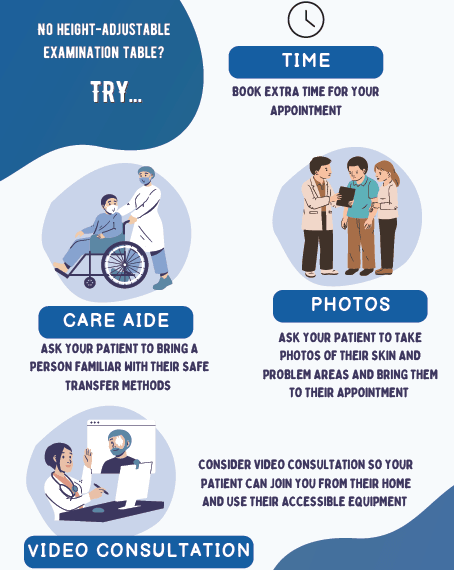
*Note: If you do not have an examination table that is height adjustable (i.e., easy for someone in a wheelchair to transfer on to), consider the following options:
- Book an extra amount of time for your patient with SCI’s appointment.
- Ask your patient to bring in a care aide or other person familiar with their safe transfer methods.
- Ask your patient to use their phone to take photos of their skin and any problems areas and bring them to the appointment.
- Consider using video consultation so your patient can join you from their home and use all of their accessible equipment for easier examination.
Ask your patient about skin health and pressure relief at every single Primary Care appointment.
Elements of a Comprehensive Skin Assessment
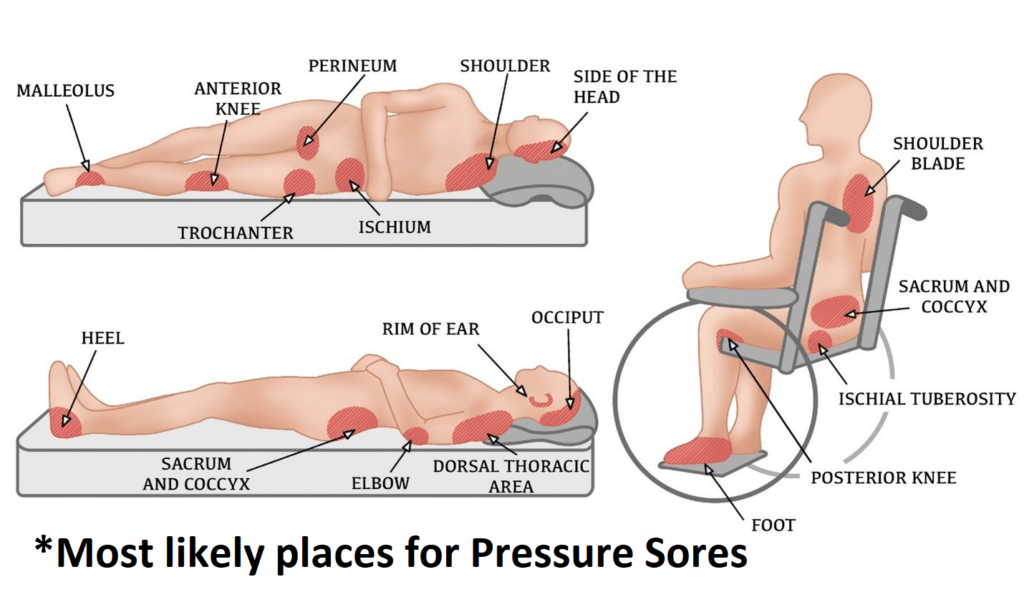
A comprehensive skin assessment entails a close observation and inspection of a patient’s entire body. This means clothing and socks should be off to fully examine a patient’s skin from front to back, head to toe, in particular to review high risk areas for pressure sores.
These include:
- Prominent bony areas – elbow, heel, shoulder blade
- Anywhere that is often touching surfaces – buttocks/sit bones, sacrum/coccyx, back of head (particularly for those with headrests on their chairs)
Preventing pressure ulcers and other skin damage is the best strategy as pressure injuries are much harder to treat than to avoid! A comprehensive skin assessment should be done early in the relationship to establish a baseline.
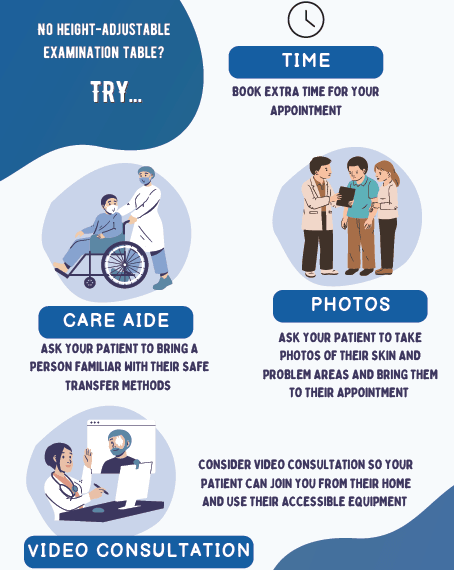
*Note: If you do not have an examination table that is height adjustable (i.e., easy for someone in a wheelchair to transfer on to), consider the following options:
- Book an extra amount of time for your patient with SCI’s appointment.
- Ask your patient to bring in a care aide or other person familiar with their safe transfer methods.
- Ask your patient to use their phone to take photos of their skin and any problems areas and bring them to the appointment.
- Consider using video consultation so your patient can join you from their home and use all of their accessible equipment for easier examination.
Generally speaking, Stage I or II PUs can be treated either in primary care or with standard wound care nursing. Stage III or IV wounds will require specialist and/or surgical intervention.
Depending on issue, referral could be to:
- Wound nurse (regular fixing of wound/changing dressings),
- Plastic surgeon (surgical repair of Stage 3 or 4 wound),
- Dermatologist (other skin issue – rash, burns, pustules, etc.)
- OT, PT, Wheelchair specialist (equipment upgrade, specialized pressure-distribution cushions, etc.),
- Dietician (better nutrition for skin health and wound healing)
Consider using telephone and video conferencing for consulting with other members of the healthcare team and to assist with follow-up, as pressure would healing may take some time.
Access to specialists (dermatology, physiatry) may be limited, particularly if you do not live in or near a major city.
Advanced screening re your patient’s skin health may best be handled by a physiatrist, occupational therapist, wound care team, or others with experience in SCI. These specialists will be essential for your patient’s health care team.
If you or your patients with SCI are not already connected, please try to gain access to a physiatrist near you. Refer to the list of SCI centers worldwide below:
- Australia (Queensland Spinal Cord Injuries Service): https://www.health.qld.gov.au/qscis
- Canada: https://praxisinstitute.org/research-care/key-initiatives/national-sci-registry/registry-sites
- Europe (enrolled in European Multicenter Spinal Cord Injury Study): https://www.emsci.org/index.php/members
- UK: https://www.brainandspine.org.uk/wp-content/uploads/2018/03/BSF_List-of-Neurocentres-in-the-UK.pdf
- USA: https://www.spinalcord.com/spinal-cord-injury-hospitals-rehabilitation-directory
(Please email SCIRE Professional if we do not have a list for your country)
- Cardenas DD, Hoffman JM, Kirshblum S, McKinley W. Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil. 2004 Nov;85(11):1757-63. doi: 10.1016/j.apmr.2004.03.016.
- LeFort M, Espagnacq M, Perrouin-Verbe B, Ravaud JF. Risk Analyses of Pressure Ulcer in Tetraplegic Spinal Cord-Injured Persons: A French Long-Term Survey.Arch Phys Med Rehabil. 2017 Sep;98(9):1782-1791. doi: 10.1016/j.apmr.2016.12.017. Epub 2017 Jan 25.
- Brienza D, Krishnan S, Karg P, Sowa G, Allegretti AL. Predictors of pressure ulcer incidence following traumatic spinal cord injury: a secondary analysis of a prospective longitudinal study. Spinal Cord. 2018 Jan;56(1):28-34. doi: 10.1038/sc.2017.96. Epub 2017 Sep 12.
- Gelis A, Dupreyon A, Legros P, Benaim C, Pelissier J, Fattal C. Pressure ulcer risk factors in persons with spinal cord injury part 2: the chronic stage. Spinal Cord. 2009 Sep;47(9):651-61. doi: 10.1038/sc.2009.32. Epub 2009 Apr 7.
- Rosin NR, Tabibi RS, Trimbath JD, Henzel MK. A Primary Care Provider’s Guide to Prevention and Management of Pressure Injury and Skin Breakdown in People With Spinal Cord Injury.Top Spinal Cord Inj Rehabil. 2020 Summer;26(3):177-185. doi: 10.46292/sci2603-177.
- Elements of a Comprehensive Skin Assessment. Developed by Boston University Research Team. Adapted from: Section 7. Tools and Resources (continued). Content last reviewed October 2014. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu7b.html From https://www.medline.com/strategies/skin-health/comprehensive-skin-assessments-correctly-get-whole-picture/
- European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. (2014). Prevention and Treatment of Pressure Ulcers : Quick Reference Guide. Clinical Practice Guideline. http://www.npuap.org/wp-content/uploads/2014/08/Updated-10-16-14-Quick-Reference-Guide-DIGITAL-NPUAP-EPUAP-PPPIA-16Oct2014.pdf
- Groah SL, Schladen, M, Pineda CG, & Hsieh CHJ. Prevention of Pressure Ulcers Among People With Spinal Cord Injury: A Systematic Review. PM&R 2015; 7(6), 613-636.
- Scovil CY, Delparte JJ, Walia S, Walia S, . . . SCI KMN Group.(2019). Implementation of pressure injury prevention best practices across 6 Canadian rehabilitation sites: Results from the spinal cord injury knowledge mobilization network. Archives of Physical Medicine and Rehabilitation, 100(2), 327-335. doi:10.1016/j.apmr.2018.07.444
- Actionable Nuggets (4th ed., 2019) – https://actionnuggets.ca/17-treatment-of-skin-breakdown/ and https://actionnuggets.ca/16-prevention-of-skin-breakdown/
- Atkinson RA, & Cullum NA.(2018). Interventions for pressure ulcers: A summary of evidence for prevention and treatment. Spinal Cord, 56(3), 186-198. doi:10.1038/s41393-017-0054-y.
- Henzel MK, Bogie KM. Medical management of pressure injuries in patients with spinal cord disorders. In: Kirshblum S, Lin V (eds.), Spinal Cord Medicine. 3rd ed. New York, NY: Demos Medical; 2019: 516-543.
- Consortium for Spinal Cord Medicine Clinical Practice Guidelines. Pressure Injury Prevention and Treatment Following Spinal Cord Injury: A Clinical Practice Guideline for Health-Care Professionals. 2nd ed. Washington, DC: Paralyzed Veterans of America; 2014.
- McInnes E, Jammali-Blasi A, Bell-Syer SE, et al. Support surfaces for pressure ulcer prevention. Cochrane Database Syst Rev. 2015;(9):CD001735. doi:10.1002/14651858.CD001735.pub5
- Edsberg LE, Black JM, Goldberg M, et al. Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. J Wound Ostomy Continence Nurs. 2016;43(6):585- 597. doi:10.1097/WON.0000000000000281
- Section 7. Tools and Resources (continued). Content last reviewed October 2014. Agency for Healthcare Research and Quality, Rockville, MD.
https://www.ahrq.gov/patient-safety/settings/hospital/resource/pressureulcer/tool/pu7b.html van Loo MA, Post MW, Bloemen JH, et al. Care needs of persons with long-term spinal cord injury living at home in the Netherlands. Spinal Cord. 2010;48(5):423–428. doi:10.1038/sc.2009.142
For Clinical Practice Guideline recommendations based on your patient’s level of injury and specific complaint, click here for the Can-SCIP Coach App.
For more information see our Skin Integrity and Pressure Injuries Module.
Disclaimer
All content and information on this website is for informational and educational purposes only, does not constitute medical advice, and does not establish any kind of patient-client relationship by your use of this website. The information here has been curated by experts in spinal cord injury treatment but it is not a substitute for actual medical consultation. Always see a medical professional directly for specific treatment for your particular needs including any professional, health-related, legal, medical, or financial decisions.