Sitting, Standing and Balance Training
Most individuals with incomplete SCI have the potential to recover some degree of mobility and many functional activities of daily living (ADL) through rehabilitation (McKinley et al. 1999). Proper balance control is important not only for mobility and ambulation, but in fact underlies daily home and community-based functional activities in sitting and standing (Huxham et al. 2001).
SCI is accompanied by changes in sensation, loss of muscle strength, decreased cognitive reserve and spasticity amongst a host of other pathological changes that may lead to balance and gait impairments. Balance and gait impairments in turn, may lead to falls. The incidence of falls in people with SCI has been reported to be as high as 75% with loss of balance being the primary perceived factor contributing to falls in incomplete SCI (Brotherton et al. 2006). Moreover, falls are a major contributor of SCI with falls being the most common cause of SCI in individuals > 60 years old (Dohle and Reding, 2011). It is not currently known the extent to which deficits in balance may affect people with SCI.
The central nervous system (CNS) maintains balance by integrating information from visual, vestibular and sensorimotor systems (Horak and Macpherson, 2006). Greater understanding of the principles underlying the neural control of movement and functional recovery following neurological injury has resulted in increased efforts to design rehabilitation strategies based on task-specific training (Wolpaw and Tennisen, 2001; Behrman and Harkema, 2007; Fouad and Telzaff, 2012). This concept has been translated to various rehabilitation interventions, such as those targeting walking outcomes (e.g. body-weight supported treadmill training) (Mehrholz et al. 2008; Van Hedel and Dietz, 2010; Wessels et al. 2010; Harkema et al. 2012) or arm and hand function (e.g. constraint-induced movement therapy) (Taub et al. 1999; Wolf et al. 2002). For balance, task specific rehabilitation similarly focuses on the achievement of the three main functional goals encompassing balance: 1) maintaining an antigravity posture such as sitting and standing, 2) anticipatory postural control during voluntary self-initiated movements and 3) reactive postural control during an unexpected perturbation (Berg, 1989).
There has been a great deal of focus on the effectiveness of gait training in SCI rehabilitation research (Mehrholz et al., 2008; Van Hedel and Dietz, 2010; Wessels et al. 2010; Harkema et al. 2012), but there has been relatively little attention on the impact of interventions specifically targeting balance outcomes. In other neurologic populations, there is some evidence that task-specific balance training can be effective for improving functional outcomes. A systematic review in people with stroke found moderate evidence that balance could be improved with exercises such as challenging static/dynamic balance ability and practice of balance in different functional tasks, including sitting, standing, walking, and stair climbing (Lubetzky-Vilnai and Kartin, 2010). In recent years, and with the rapid development in technology (e.g., exoskeletons, virtual-reality), there has been more data available about balance outcomes following gait training (Dobkin et al. 2006; Wu et al. 2012; Harkema et al. 2012), as well as specific sitting (Boswell-Ruys et al. 2010; Harvey et al. 2011) or standing (Alexeeva et al. 2011) balance interventions in people with SCI.
Sitting Balance
Acute (< 6 months) SCI
One good quality RCT examined the effect of an additional 3 weeks of task specific exercises on sitting balance in individuals with acute SCI following 6 weeks of standard inpatient rehabilitation consisting of practice of activities of daily living (N=32, AIS A=29, AIS B=2, AIS C=1) (Harvey et al. 2011). Participants were mainly motor complete paraplegics with a median time since injury of 11 weeks. Both experimental and control groups received 6 weeks of standard inpatient rehabilitation consisting of practice of activities of daily living. Despite receiving more training sessions, there was no additional benefit to the experimental group compared to the control group on functional outcomes of sitting balance.
Chronic (> 1 year) SCI
There were 5 studies that investigated the effects of various interventions (i.e. kayak ergometry, task specific exercises in unsupported sitting) on sitting balance. The majority of the participants had motor-complete SCI (N=76, AIS A=51, AIS B=23, AIS C=2). Sitting balance was significantly improved with kayak ergometer training in two Level 4 evidence trials with substantial transfer effects to functional tests in the wheelchair (Bjerkefors and Thorstensson, 2006; Bjerkefors et al. 2007). No significant effect was reported of 8 weeks open water kayak training vs. able-bodied control group who did not train (Grigorenko et al. 2004).
A good quality RCT assessed sitting balance in chronic SCI using the same task specific exercises as the study by Harvey et al (Harvey et al. 2011) in unsupported sitting for 6 weeks vs. a control group who received no training (N=30, AIS A=25, AIS B=15) (Boswell-Ruys et al. 2010). Overall improvements in both the training and control groups were reported. The addition of task-specific exercises using a rocker board to conventional physical therapy for 4 weeks yielded significant improvements in sit and reach tests as well as COP measures (N=12, AIS A=11, AIS B=1) (Kim et al. 2010). However, this was a relatively small study (N = 12) and it did not appear that participants were randomly assigned to the interventions.
Standing Balance
Acute (< 6 months) SCI
There was one lower quality RCT that compared BWSTT (experimental group) vs. over ground gait training (control group) in acute (<8 weeks post-injury) incomplete SCI (N=146, N=45 at 6 months; AIS C=38, AIS D=7, 12 weeks of training) (Dobkin et al. 2006) (Table 3). There were no significant differences in balance scores following training between the two groups. However, there was a large median difference between baseline and 6-months post-training in both groups, indicating that for people who were able to walk at six months (N=45), both types of interventions resulted in considerable improvements in balance scores.
Chronic (> 1 year) SCI
Virtual Reality
There were 3 trials that assessed standing balance in people with chronic incomplete SCI using virtual reality (VR) (N=38, AIS C=6, AIS D=20, Table 3). Two studies performed similar VR interventions consisting of standing on a force plate and performing task specific exercises while the center of pressure (COP) position signal was used for visual biofeedback for 4 and 8 weeks respectively (Sayenko et al. 2010; Tamburella et al. 2013). Pre-post studies support the feasibility and reported positive effects on balance function using this approach (Sayenko et al. 2010; Villiger et al. 2013). In the study by Tamburella et al, participants were randomized to receive active training with or without the visual biofeedback. After 8 weeks of training, only the experimental group showed significant improvements in BBS (Baseline= 26.0±10.69 to post-training=41.0±7.8) and Timed Up and Go test (Baseline=21.70±10.70 to post-training=15.22±6.14) (Tamburella et al. 2013).
Body Weight Support Training (BWST)
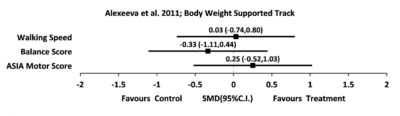
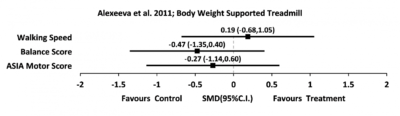
There were 4 trials that measured standing balance in incomplete SCI following body-weight supported treadmill training. One good quality RCT (Alexeeva et al. 2011), and three studies of level 4 evidence (Musselman et al. 2009; Fritz et al. 2011; Wu et al., 2012) utilized BWST in addition to various interventions such as treadmill, over ground, physical therapist (PT) skills training or a combination of these. After 8 weeks of training, PT skills training resulted in greater balance improvements than BWSTT and BWST on a track (Alexeeva et al. 2011). Small to medium effect sizes for the BBS (0.31-0.67) were reported when BWST was combined with 10 days of intensive mobility training (Fritz et al. 2011). An overall improvement in BBS was found when combining 8 weeks of BWSTT with resistance or assistance but no significant difference between the 2 interventions was reported (Wu et al., 2012).
Four level 4 evidence pre-post trials from the same clinical setting spanning reported significant improvements in balance scores following a program of 3-5 days per week of treadmill- progressing to overground-based BWST (NRN protocol; Behrman et al. 2012; Buehner et al. 2012; Harkema et al. 2012; Lorenz et al. 2012). In addition, this data set demonstrated that the Berg Balance Scale scores were significantly correlated to the severity of injury (Lorenz et al. 2012). Among the pre-post studies, effect sizes were generally small for interventions involving BWST regardless if they were combined with other types of therapy when assessed using the BBS (d=0.18-0.47) with the exception of 1 case-control trial (d=0.88) (Musselman et al. 2009).
There are some drawbacks of measuring balance with only functional outcomes. A ceiling effect was observed in BBS scores of SCI participants receiving BWST with assistance and resistance (Wu et al. 2012). Only one trial was able to use predictable and unpredictable perturbations to assess balance reactions after kayak ergometry training (Bjerkefors et al. 2007). Nonetheless, functional measures are quick, cost effective and easy to apply in both the research and clinical setting and have the added benefit of being validated for the SCI population (Lemay and Nadeau, 2009). It would be optimal that when assessing balance, where feasible, reactions to sudden movements are included in order to give a more comprehensive understanding of balance capacity in persons with SCI.
Conclusion
Only preliminary recommendations can be made from the results of this review as there are relatively few studies that provide information on specific balance outcomes in SCI. Early balance training does not appear to enhance the effects of standard physical therapy in either sitting or standing balance. In people with chronic SCI who cannot stand, sitting balance can be improved with both static and dynamic task specific training. For participants with lower severity injuries (e.g., AIS C and D), BWS over ground training combined with physiotherapist-led task-specific exercises and feedback appear to be more effective to improve standing function than BWSTT alone.
There is Level 2 evidence (Dobkin et al. 2006) that there were no differences in balance whether participants engaged in overground training or Body-weight supported treadmill training, but the participants that completed either training and were able to walk made considerable progress in balance.
There is Level 4 evidence (Sayenko et al. 2010; Tamburella et al. 2013) that visual field feedback training leads to substantial improvements in static and dynamic standing eyes open and closed scores, and improvements in balance performance during training-irrelevant tasks.
Tamburella et al. found that the visual biofeedback task specific balance training group saw improvements in balance and gait, and that it demonstrated a significantly higher level of effectiveness than conventional rehabilitation.
There is one study with Level 1 evidence (Alexeeva et al. 2011) and 3 studies with Level 4 evidence (Musselman et al. 2009; Fritz et al. 2011; Wu et al., 2012) that found that BWSTT in addition to Physical Therapy resulted in greater balance improvements than BWSTT alone. Wu et al. found non-significant differences in balance when combining BWSTT with resistance or assistance training.
There is Level 4 evidence (Behrman et al. 2012; Buehner et al. 2012; Harkema et al. 2012; Lorenz et al. 2012) that treadmill and overground based BWST leads to improvements in balance scores.
There is level 1 evidence (Harvey et al. 2011) that task-specific sitting balance exercises for an additional 3 weeks in acute SCI resulted in no difference on balance outcomes.