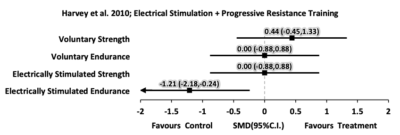
| Harvey et al. 2010
Australia
PEDro=10
RCT
Level 1
N=20 |
Population: Complete or incomplete SCI patients
Experimental group – 7 males, 3 females; mean age 40; mean YPI 3
Control group – 7 males, 3 females; mean age 39; mean YPI 4.Treatment: ES superimposed on PRT 3 days/week for 8 weeks (12 sets of 10 knee extension repetitions against increasing resistance, the first 6 using ES and voluntary contraction and the second 6 using only ES).
Outcome Measures: Quadriceps strength and endurance, the performance and satisfaction scales of the Canadian Occupational Performance Measure (COPM), the ES-evoked quadriceps strength (Nm), ES-evoked quadriceps endurance (fatigue ratio), participant perception of treatment effectiveness. |
- There was a statistically significant group differences for voluntary quadriceps strength change (14 Nm), but the magnitude may not be clinically important.
- ES group had greater perception of treatment effectiveness over control.
- There was no group difference in any other variables.
|
| Effect Sizes: Forest plot of standardized mean differences (SMD ± 95%C.I.) as calculated from pre- and post-intervention data
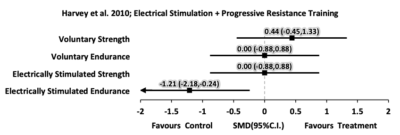
|
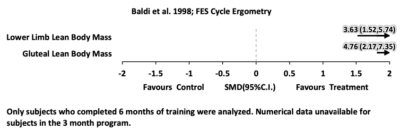
| Baldi et al. 1998
USA
PEDro=5
RCT
Level 1
N=26 |
Population: 26 males and females; age 25-28 yrs; traumatic motor complete; cervical or thoracic lesion level; 15 wks post-injury.
Treatment: Random assignment to 3-6 months of 1. FES-assisted cycle ergometry (n=8), 30 min, 3X/week; 2. PES-assisted isometric exercise group (n=8) (same muscle groups as FES group) for 1 hr, 5X/week and 3 control group (n=9) with no stimulation.
Outcome Measures: lean body mass lower limb. |
- Lean body mass increased with FES-cycling at all regions and declined for control and PES group.
- With respect to total body lean mass, lower limb lean mass and gluteal lean mass, controls lost an average of 6.1%, 10.1%, 12.4% after 3 months and 9.5%, 21.4%, 26.8% after 6 months.
|
| Effect Sizes: Forest plot of standardized mean differences (SMD ± 95%C.I.) as calculated from pre- and post-intervention data
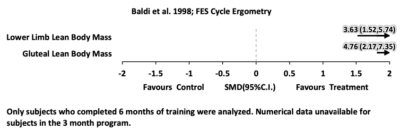
|
| Shields & Dudley-Javoroski 2006
USA
Prospective Controlled Trial
Level 2
N=7 |
Population: 7 males; age 21-43 yrs; AIS A; C5-T10 lesion level; ³ 6 weeks post-injury
Treatment: PES exercise to unilateral ankle plantarflexion (untrained leg served as a control). Four 4 min exercise bouts, 5 days/week for 1.87-3.05 years.
Outcome Measures: Stimulated ankle torque and soleus twitch profiles at baseline and every 6 months up to 3 years. |
- Compared to the untrained side, stimulated limb had:
- Increased strength (increased peak stimulated ankle torque and higher torque-time integrals).
- More resistant to fatigue (increased muscle fatigue indexes).
- Increased twitch difference (indicative of force generating capacity), especially with successive stimulation trains.
|
| Ryan et al. 2013
USA
Pre-post
Level 4
N=14 |
Population: 14 participants with chronic motor complete SCI (11M 3F); 2 diabetic. Inclusion criteria included: 18-65 yrs of age; AIS A or B classification; normative range of motion in the knee and hip joints.
Treatment: Participants performed RET of the knee extensor muscles 2 times/week for 16 weeks. 4 sets of 10 knee extensions were performed using NMES.
Outcome Measures: Plasma glucose and insulin throughout a standard clinical oral glucose tolerance test; thigh muscle and fat mass via dual-energy x-ray absorptiometry; quadriceps and hamstrings muscle size and composition via MRI; muscle oxidative metabolism using phosphorus magnetic resonance spectroscopy. |
- After RET, thigh fat tissue (g), thigh percentage fat and bone mineral density of the femur bone was not different. Lean tissue of the thigh area increased by approximately a mean(SD) of 10(15)%g.
- Quadriceps muscle volume (average of both legs) was increased by 39(27)% after RET (pre vs post: 618(343) vs 815(399) cm3). No change was observed in absolute fat volume for either the quadriceps or hamstring muscles. No relation was found between the magnitude of muscle hypertrophy and improvements in glucose or insulin status.
- 8 participants had measurements of PCr recovery kinetics. Time constants for the recovery of PCr after electrical stimulation were 102(24) and 77(18) seconds before and after RET; this represents an approximate 25% improvement in skeletal muscle oxidative capacity, which was statistically significant.
|
| Sabatier et al. 2006
USA
Pre-post
Level 4
N=5 |
Population: 5 males; mean (SD) age 35.6(4.9) yrs; complete; C5-T10 lesion level; 13.4(6.5) yrs post-injury
Treatment: 18 weeks of neuromuscular electrical stimulation resistance training for the quadriceps combined with additional weight around the shin, 2x/week with 4 sets of knee extensions.
Outcome Measures: Weight lifted, muscle mass, muscle fatigue |
- All participants increased weight lifted during training by an average (SD) of 6.9(1.4) kg
- Significant increases in cross-sectional area of quadriceps femoris in both thighs (right mean CSA increased from 32.6 to 44.0 cm2, left mean increased from 34.6 to 47.9 cm2)
- Progressive decrease in fatigue throughout training and after 18 weeks of training. Decreases significantly at 12 weeks and 18 weeks.
|
| Belanger et al. 2000
Canada
Pre-post
Level 4
N=14 |
Population: 14 males and females; age 23-42 yrs; 2 incomplete, 12 complete lesions; C5-T5 lesion level; 1.2-23 yrs post-injury
Treatment: Bilateral functional electrical stimulation to quadriceps combined with isokinetic resistance training on left side and unresisted on right; 5 days/week, 24 weeks; each session was 1 hr or until fatigue
Outcome Measures: knee torque, endurance |
- Average increase in knee extensor muscle torque on resisted side was 150% (average 8.1% increase/week)
- Average increase in knee muscle torque on unresisted side was 75% (average 4.5% increase/week)
- No change in endurance (fatigability)
|
| Kagaya et al. 1996
Japan
Pre-post
Level 4
N = 5 |
Population: 5 males; age 19-68 yrs; with complete paraplegia (T5-L2 lesion level); 3-60 months post-injury.
Treatment: Subcutaneous PES to various lower limb nerves and muscles for 6 months. Applied at 10 min, 3X/day and gradually increased to 60 min, 3X/day at 10 weeks.
Outcome Measures: Muscle cross-sectional area (CT scan), manual muscle test, stimulated muscle torque. |
- No group statistical analysis performed, limited by heterogeneity across participants.
- All cross-sectional muscle areas except gluteus maximus increased significantly.
- Muscle torques generally increased after PES.
- Manual muscle tests generally increased significantly for muscles that initially graded as poor-minus (no voluntary movement against gravity).
|
| Hjeltnes and Lannem 1990
Norway
Pre-post
Level 4
N=4 |
Population: 4 males and females; age 20-36 yrs; Frankel A; T5-T12 lesion level; 3 mos-5 yrs post-injury
Treatment: PES, 4 weeks, 2x/day, 5-10mins, isokinetic resistance to quadriceps muscles followed by 4 weeks, 30 min, 2X/day, 4-5X/day of integrated training of rising and standing.
Outcome Measures: Knee extension torque, thigh circumference, CK, collected monthly. |
- No group statistics done. At least 2 participants had increased knee extension torque, increased muscular endurance, increased thigh circumference, increased CK (indicator of muscle injury). The more acute participant stopped training due to muscle spasms.
- One participant progressed to the planned stage of FNS-assisted ambulation training.
|
| Gerasimenko et al. 2015
Russia
Post-test
Level 4
N=10 |
Population: 10 individuals- 5 able bodied and 5 with SCI.
Treatment: Painless transcutaneous electrical enabling motor control (pcEmc) neuromodulates the physiological state of the spinal cord. This method includes electrically activating the spinal circuitry via electrodes placed on the skin overlying the vertebrae of the lower thoracic and/or lumbosacral vertebrae. This waveform consists of 0.3- to 1.0-ms bursts with a carrier frequency of 10 kHz administered at 5 to 40 Hz. PcEmc stimulation was delivered by a 2.5-cm round electrode placed midline at the C5, T11, and/or L1 spinous processes as cathodes and two 5.0 10.2 cm2 rectangular plates made of conductive plastic placed symmetrically on the skin over the iliac crests as anodes. Biphasic rectangular 0.5- to 1.0-ms pulses with a carrier frequency of 10 kHz and at an intensity ranging from 30 to 200 mA were used.
Outcome Measures: EMG amplitude |
- Use of the multielectrode surface array can fine-tune the control of the locomotor behavior.
- The pcEmc strategy combined with exoskeleton technology is effective for improving motor function in paralyzed patients with SCI.
|