Epidural Stimulation
Epidural stimulation has emerged in the literature on spinal cord injury and may present a new method for managing symptoms of SCI. Epidural stimulation is a form of FES that uses electrical currents on the lower spinal cord to stimulate the nerves and elicit muscle contractions. An electrode is placed in the epidural space behind the spine and electrical currents are sent directly to the bypassing brain-to-spinal cord pathways to help reactivate remaining intact neural networks that may facilitate the movements to stand and walk, for example.
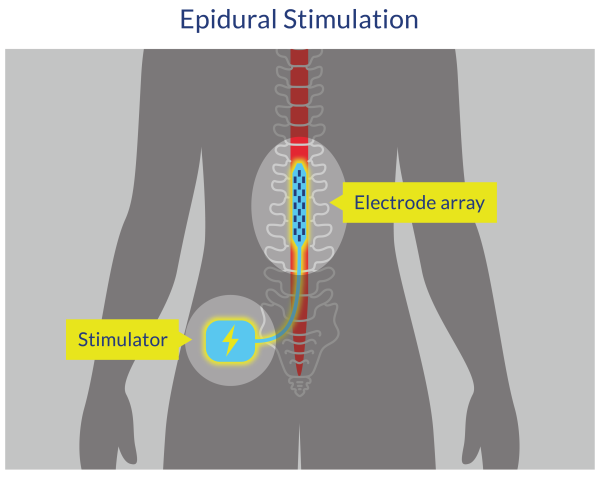
Figure 4. Epidural Spinal Cord Stimulation
Discussion
Two prospective studies examined the effect of scES on blood pressure in individuals with SCI and neither found sufficient evidence to suggest that scES could attenuate or remove episodes of AD (Herrity et al. 2021; Pino et al. 2022). Herrity et al. (2021) did not observe differences in sBP in response to bladder distention following ABRT-scES; however, participants receiving ABRT-scES had lower sBP responses to bladder distention post-training compared to those in usual care. On the other hand, Pino et al. (2022) found no differences in sBP between supine to head-up-tilt (HUT) and HUT with scES. Furthermore, there was no increase in frequency or severity of AD with the application of scES, although 2 of the 10 participants experienced elevations in sBP enough to represent AD (> 150 mmHg for ≥30) (Pino et al. 2022).
On the other hand, a case series by Samejima et al. (2023) found the application of eSCS to prevent AD during digital anorectal stimulation (DARS), with each participant experiencing only a marginal elevation in sBP that does not meet the threshold for AD diagnosis.
Evidence is too preliminary at this time to support or deny the use of scES for AD management in people with SCI. However, Herrity et al. (2021) suggest that the training effect found in their study supports the role of intersystem stimulation; that integrating an scES protocol for both bladder and cardiovascular function could improve responses to bladder distention.
Conclusion
There is level 2 evidence (from one prospective controlled trial) (Herrity et al. 2021) that elevated blood pressure elicited during bladder distention was not attenuated with ABRT-scES, but post-training, the ABRT-scES group had significantly lower sBP responses than the usual care group during bladder distention.
There is level 2 evidence (from one prospective cohort study) (Pino et al. 2022) that scES does not increase the frequency of severity of AD, although 2 of 10 participants experienced elevations of sBP enough to represent an episode of AD (> 150 mmHg for ≥30 s).
There is level 4 evidence (from one case series) (Samejima et al. 2023) that the application of eSCS prevents AD during digital anorectal stimulation.
