Mechanical Ventilation
One of the most important avenues of respiratory management is MV. There have been increases in the incidence of high-level cervical SCI and incomplete traumatic cervical SCI, resulting in a greater percentage of ventilator-dependent patients (McCaughey et al. 2016a; Montoto-Marqués et al. 2018). Patients can be ventilated with non-invasive mask ventilation or more invasive endotracheal or transtracheal (with a tracheostomy) ventilation. Often these more invasive procedures are needed to allow for suctioning excess secretions to prevent the development of complications such as atelectasis or pneumonia (Gregoretti et al. 2005). Patients may experience more than one type of ventilation during their hospital stay as their needs adjust (i.e., they may initially be intubated with endotracheal ventilation and later proceed to transtracheal intubation to assist in ventilator weaning).
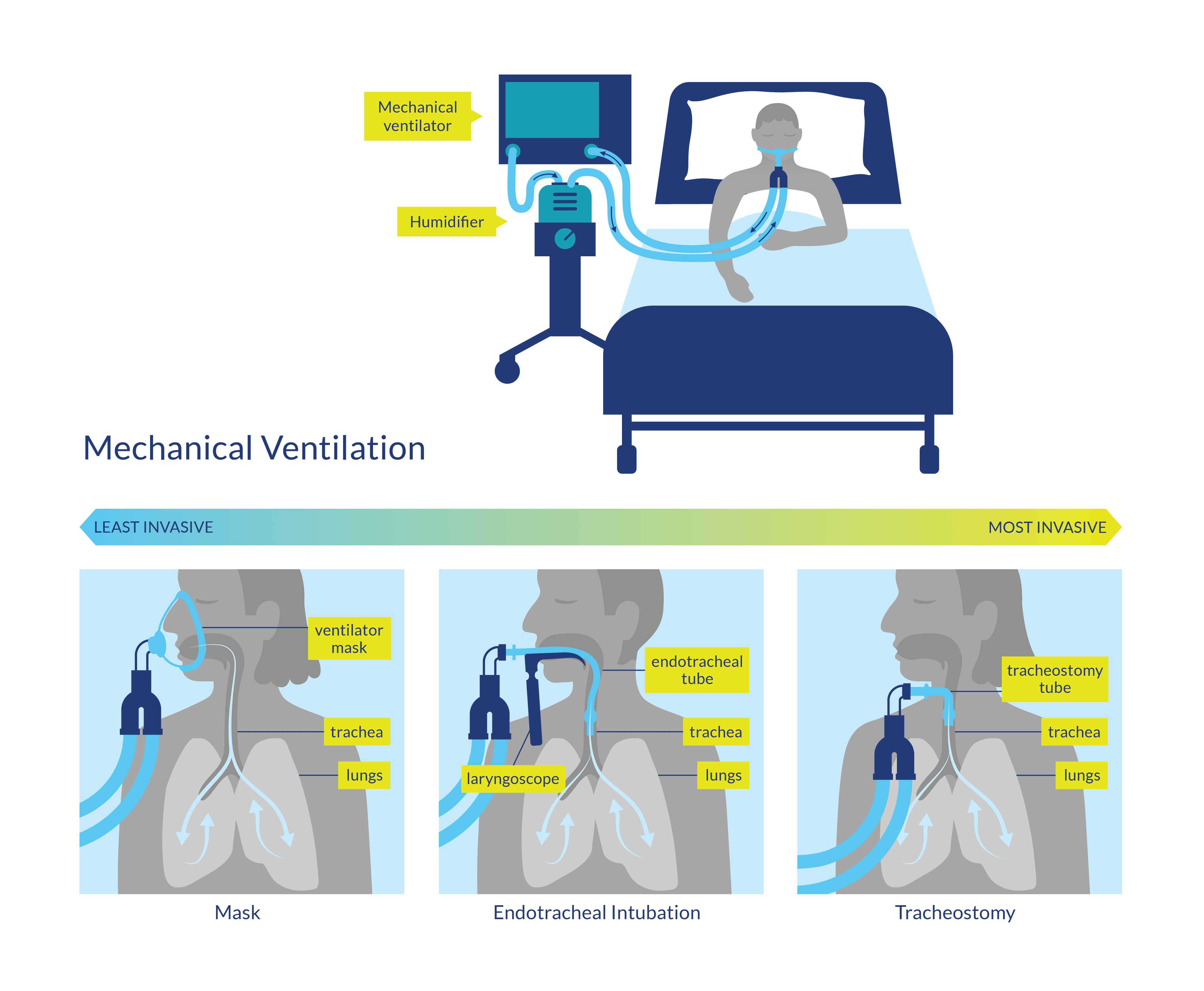
Figure 1. Mechanical ventilation procedures
There are several modes of ventilation used for patients that vary in the amount of volume or pressure controlled based on pre-set variables to maximize lung function. For example, intermittent positive pressure breathing is one of the oldest ventilation strategies in which all inspirations are provided through the application of positive pressure to the airway. Its use is common in patients with acute SCI, yet its general efficacy is still largely unknown (Denehy & Berney 2001) and is understudied in the SCI population. Intubation for MV often occurs at the time of injury to manage respiratory failure or to protect the airway in cases of complete SCI between C1 and C5 (Berney et al. 2011). In contrast, incomplete injuries lower than C5, where the airway is not immediately compromised or at risk, ventilation is often still initiated approximately four days after injury when levels of carbon dioxide rise in the blood due to difficulty expiring (Galeiras Vázquez et al. 2013). Although ventilatory needs are unique for each patient, it is useful to determine which factors predict the need for MV in an effort to develop practice guidelines and reduce overall hospital stay (Casha & Christie 2011).
One observational study found, not unexpectedly, that patients with ASIA grades A and B were more likely to require MV, as well as those with higher injury severity scores (Montoto-Marques et al. 2018). Other factors include complete injuries, high Injury Severity Score (ISS), and compound injuries (Velmahos et al. 2003; Como et al. 2005; Seidl et al. 2010).
