Upper Extremity Exercise
Given the motor loss of the lower limbs following injury, upper extremity exercise is a logical choice for improving cardiovascular fitness and health. However, improving cardiovascular function can be challenging using the smaller mass of the arms especially when muscle fatigue can often occur before exercise training targets are met. From our search, we found five RCTs, two high quality (de Groot et al. 2003; Ordonez et al. 2013), and three lower quality trials (Davis et al. 1987; Davis et al. 1991; Hicks et al. 2003), two prospective controlled (Hooker and Wells 1989; Hjeltnes and Wallberg-Henriksson 1998), a case report (Tordi et al. 2009), a case-controlled investigation (Jae et al. 2008), one cohort study (Valent et al. 2008), and 20 pre-post studies.
Given the large number of studies that have looked at upper extremity exercise, we have tabled only those studies that included a control group consisting of participants with SCI (Table 5).
Discussion
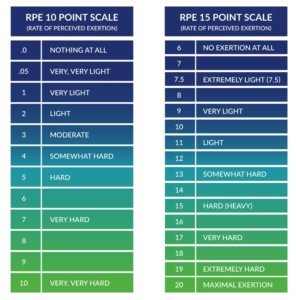
The reported improvements in aerobic capacity after aerobic arm training in SCI are approximately 20%–30%; however, it is not uncommon for improvements in excess of 50% (DiCarlo 1988). The majority of aerobic training investigations have evaluated the effectiveness of moderate (40%–59% heart rate reserve (HRR) or 55%–69% of maximum HR) to vigorous (60%–84% HRR or 70%–89% of maximum HR) intensity exercise. These studies have used arm ergometry, wheelchair ergometry, and swimming-based interventions. Based on the current level of literature, it appears that moderate intensity exercise performed 20–60 minutes per day for at least three days/week for a minimum of six weeks is effective for improving cardiovascular fitness and exercise tolerance in persons with SCI (Level 1b evidence based on two high-quality RCT’s (Ordonez et al. 2013; de Groot et al. 2003) and several lower quality RCTs). Therefore, the general recommendations provided by many international agencies (i.e., 150 min of moderate-to-vigorous physical activity (Tremblay et al. 2011) are appropriate for improving the cardiovascular fitness of persons with SCI. However, these recommendations are not optimal as significant changes in aerobic fitness may occur at volumes of exercise well below international recommendations designed for apparently healthy individuals (Ginis et al. 2011). It is also important to note that training intensities may need to be established using a rating of perceived exertion (e.g., RPE) (rather than objective measures of heart rate) in individuals with SCI-induced autonomic denervation of the heart.
An exercise intensity threshold of 70% maximal HR reserve has been advocated for the attainment of training benefits when exercising for the standard 20 minute duration (Hooker and Wells 1989; Tordi et al. 2001; Bizzarini et al. 2005). It is also apparent that improvements in exercise capacity and functional status may occur after training without significant changes in VO2peak, particularly in persons with tetraplegia (Hjeltnes and Wallberg-Henriksson 1998).
Questions remain regarding the primary mechanisms for improvements in aerobic fitness after training. It is unclear whether central (heart and lung) or peripheral (skeletal muscle) adaptations are of key importance. Enhancements have been observed in peripheral muscle function. For instance, investigators have shown intrinsic cellular adaptations in the paralyzed muscle that facilitate oxidative metabolism following BWSTT (Stewart et al. 2004). Only limited investigations, however, have shown an improvement in cardiac function after upper extremity aerobic exercise training (Davis et al. 1987). It could therefore be argued that peripheral adaptations are of primary importance to the improvement in aerobic capacity after this type of aerobic exercise aerobic exercise. However, this statement is somewhat misleading as the majority of studies have not directly evaluated cardiac output during maximal/peak exercise. This is owing to the fact that the assessment of maximal cardiac output during exercise is one of the most difficult procedures in clinical exercise physiology (Warburton et al. 1999a, 1999b). When exercise measures of cardiac function have been taken, improvements in central function have been observed (Davis et al. 1987). Further research examining the primary mechanism(s) of importance for the improved cardiovascular fitness and exercise capacity seen in persons with SCI after aerobic exercise training is warranted. It is also important to highlight that it is often difficult for patients to attain VO2max during exercise. Moreover, the submaximal prediction of VO2peak (based on the heart rate response to exercise) is limited owing to the potential impairment in the sympathetic drive to the heart in many persons with SCI. Furthermore, it is often difficult to determine whether the changes in VO2peak/VO2max seen after training are related to changes in musculoskeletal fitness rather than changes in cardiovascular fitness.
Less is known about the effects of resistance training on cardiovascular fitness. However, the incorporation of resistance training into the treatment of SCI appears to be essential. In fact, muscle weakness and dysfunction are key determinants of pain and functional status in persons with SCI. Previous studies have revealed improvements in maximum aerobic power (Cooney & Walker 1986; Jacobs et al. 2001), exercise tolerance (Jacobs et al. 2001), and musculoskeletal fitness (Jacobs et al. 2001) after resistance training (e.g. circuit training).
As reviewed systematically by Phillips et al. (2011) two papers have evaluated the effects of upper body (arm) exercise on arterial function in SCI (Jae et al. 2008; Tordi et al. 2009). Jae et al. (2008) revealed that there were no significant differences in intima-media thickness, compliance, and beta stiffness index (a measure of arterial elasticity) of the common carotid artery between 28 competitive SCI athletes and 24 age-matched recreationally active able-bodied controls. Tordi and colleagues (2009) revealed (in a case study) that there was an improvement in aortic pulse wave velocity (central aortic stiffness) following six weeks of upper body training (30 min/session, 3 sessions/wk).
Conclusion
There is level 1b (Ordonez et al. 2013) and Level 2 evidence (Davis et al. 1987) that moderate intensity aerobic arm training (performed 20–60 min/day, three days/week for at least 6-8 weeks) is effective in improving the aerobic capacity and exercise tolerance of persons with SCI.
There is level 1b evidence (de Groot et al. 2003) that vigorous intensity (70%–80% HR reserve) exercise leads to greater improvements in aerobic capacity than moderate intensity (50-60% HR reserve) exercise. It should be noted that many individuals with SCI cannot tolerate vigorous intensity initially, to which they must adapt often using a submaximal or interval type approach.
There is level 2 evidence (Milia et al. 2014) that arm cranking against a workload corresponding to 60% of WMax (performed 3-5 hours/day for one year) increases WMax and VO2 max.
There is level 2 evidence (Hjeltnes and Wallberg-Henriksson 1998) that hand cycling exercise increases the power output, oxygen consumption, and muscle strength in individuals with paraplegia, but not tetraplegia during active rehabilitation. Conversely, there is level 4 evidence (Valent et al. 2008) that hand cycling increases power output and oxygen consumption in individuals with tetraplegia. Further research is clearly warranted. There is also level 4 evidence (Nooijien et al. 2015) that hand cycling interval training program increases peak power output and peak VO2 in individuals with paraplegia and tetraplegia.
There is level 3 evidence (Jae et al. 2008) that upper body strength exercise training can improve arterial structure and function in those with SCI.
There is level 5 evidence (Hubli et al. 2014) that aortic pulse wave velocity is significantly lower in athletes (hand cyclists) compared to sedentary individuals with SCI.
