Treadmill Training
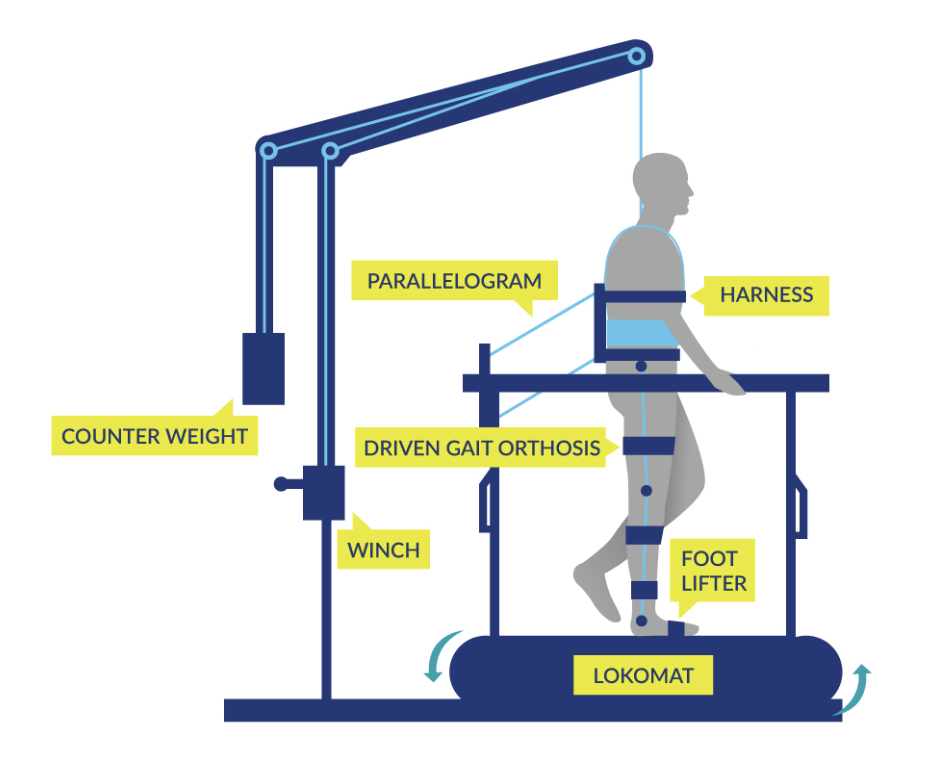
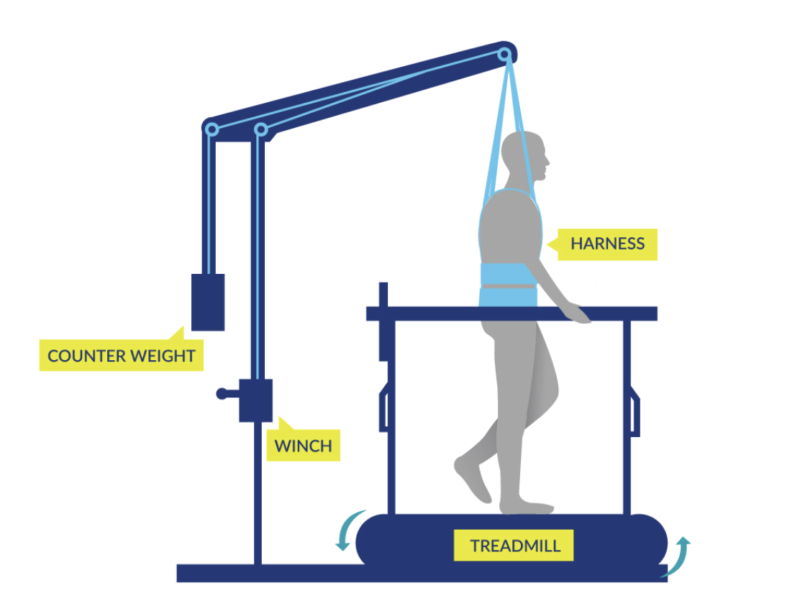
Body-weight–supported treadmill training (BWSTT) is an exercise protocol that has been used to potentially affect a number of domains, including motor recovery, bone density, cardiovascular fitness, respiratory function, as well as quality of life. Traditional BWSTT involves the upright walking on a motor-driven treadmill while a harness (suspended from an overhead pulley system) supports the participant’s body weight. Therapists conducting the session determine the magnitude of off-loading of an individual’s body weight (Phillips et al. 2004). The treadmill velocity, the amount of body weight supported, and time spent on the treadmill can be individualized (Phillips et al. 2004). Significant resources are often required as the majority of individuals will require one or two assistants to manually help ambulate the lower limbs.
For a more extensive consideration of BWSTT, please visit the section on Lower Limb, Balance and Walking chapter.
Discussion
There are two randomized controlled trials (Level 1a) (Millar et al. 2009; Alexeeva et al. 2011), and one prospective controlled investigation (Level 2) (de Carvalho et al. 2006) and several pre-post studies (Level 4) have been conducted to examine changes in indicators of cardiovascular fitness/health in SCI after training (de Carvalho & Cliquet, 2005a; Ditor et al. 2005a; Ditor et al. 2005b; Jack et al. 2009; Soyupek et al. 2009; Turiel et al. 2011).
Four recent investigations examined the effects of BWSTT (Jeffries et al. 2015; Alexeeva et al. 2011; Turiel et al. 2011) and underwater treadmill training (Stevens and Morgan 2015) on indicators of cardiovascular fitness and/or health. Alexeeva et al. (2011) compared participants randomly assigned to two different BWS ambulation modalities in comparison to traditional physical therapy, and revealed that there were clinically important improvements in normalized VO2 peak in each group. Turiel et al. (2011) demonstrated that 6 weeks of BWSTT resulted in improvements in resting left ventricular function, coronary blood flow reserve and inflammatory status.
In 2009, Jack et al. examined two participants (with thoracic injuries) after BWSTT and revealed significant improvements in peak heart rate (HR) and oxygen consumption (VO2), and a decrease in the dynamic oxygen cost (the rate of oxygen consumption by respiratory muscles as they ventilate the lungs). Soyupek et al. (2009) evaluated 8 subjects and found significantly lower heart rate post-training and improved forced vital capacity (maximum amount of air that can be expelled after maximal inhalation) and inspiratory capacity.
Stevens and Morgan (2015) examined the effects of 8 weeks of progressive and individualized underwater treadmill training (3 days per week, 3 walking trials per session). They revealed evidence of improved cardiovascular control and function (i.e., reduced submaximal HR) across the training intervention.
The two earlier studies were conducted by the same Canadian research group (Ditor et al. 2005a; Ditor et al. 2005b). They reported that BWSTT did not have substantial group effects on HR and blood pressure in motor-complete subjects but did reveal a significant reduction in resting HR in the study that involved individuals with incomplete tetraplegia. There was also evidence that improvements in HR and blood pressure variability may occur after BWSTT in incomplete SCI and a subset of participants with complete SCI. The authors attributed the change in blood pressure variability to reductions in sympathetic tone to the vasculature. These findings have significant physiological relevance since it indicates that both parasympathetic outflow to the heart (as evaluated by heart rate variability) and sympathetic flow to the vasculature (as evaluated by blood pressure variability) can adapt in response to exercise training. This research group also revealed the potential for improvements in vascular health (e.g. arterial compliance) after BWSTT in individuals with motor-complete SCI. There was no indication of the effects of BWSTT on peak oxygen consumption (VO2peak).
The mechanisms responsible for the improvement in markers of cardiovascular health and regulation in individuals with incomplete SCI remain to be determined. Jack et al. (2009) postulated that an improvement in walking ability likely explained the increase in VO2peak with training (in individuals with incomplete SCI). They also highlighted how marked atrophy, fast fatiguing lower limbs and limited neural control may limit the capacity of patients with SCI to make use of their cardiovascular reserve.
Ditor et al. (2005a,b) attributed the training-induced changes in autonomic function to the cardiovascular challenge provided by the upright nature of BSWTT (which potentially could be a sufficient stimulus in individuals with postural hypotension) and the spasticity created during the treadmill training. However, it should also be noted that both weight bearing and the passive movement of the limbs may contribute to the observed changes in these studies.
A recent Canadian study employing a randomized cross-over design (Millar et al. 2009) revealed that short-term (4 weeks) BWSTT (but not head-up tilt training) led to a significant increase in HR complexity and reduced fractal scaling distance score in persons with SCI. These changes are thought to reflect an improvement in cardiac autonomic balance after short-term BWSTT.
Two investigations (a pre-post study (level 4) and a prospective controlled study (level 2) from the same research group used partial BWSTT (30%–50%) via neuromuscular electrical stimulation assisted by physiotherapists (de Carvalho & Cliquet 2005a; de Carvalho et al. 2006). The first investigation revealed that three months of this form of gait training can result in a significant increase in systolic blood pressure at rest and during gait exercise in males with tetraplegia (de Carvalho & Cliquet 2005b). In the latter study (de Carvalho et al. 2006) the authors revealed that long-term neuromuscular electrical stimulation gait training (six months) resulted in significant increases in VO2 (36%), minute ventilation (30.5%), and systolic blood pressure (4.8%) during the gait phase. The authors concluded that treadmill gait training combined with neuromuscular electrical stimulation leads to increased metabolic and cardiorespiratory responses in persons with complete tetraplegia.
In a comparison of trials using BWSTT, an interesting discrepancy arises. For instance, in the work of Ditor et al. there was no change in resting blood pressure after BWSTT in individuals with complete or incomplete SCI (Ditor et al. 2005a; Ditor et al. 2005b). Whereas, the work by de Carvalho and coworkers revealed an increase in resting blood pressure following partial BWSTT (with neuromuscular electrical stimulation) (de Carvalho & Cliquet 2005b; de Carvalho et al. 2006). It is not clear why these discrepancies exist, and, as such, further research is clearly warranted.
It is important to note that while BWSTT may have important cardiovascular benefits, the feasibility of using this treatment over the long term in the home setting is questionable due to the costs of the equipment and assistants to set up the individual and facilitate the leg motions.
Conclusion
There is level 1a evidence (Millar et al. 2009) that BWSTT improves cardiac autonomic balance in persons with tetraplegia and paraplegia (with similar results for varying degrees of lesion level and severity).
There is multiple level 4 evidence (Jack et al. 2009; Soyupek et al. 2009) that BWSTT increases peak oxygen uptake and heart rate, and decreases the dynamic oxygen cost for persons with SCI.
There is Level 2 evidence (Jeffries et al. 2015) that indicates that standing and stepping exercises with BWSTT can increase VO2 and heart rate levels.
There is Level 4 evidence (Ditor et al. 2005b) that indicates that BWSTT can improve arterial compliance in individuals with motor-complete SCI.
There is Level 4 evidence (Stevens & Morgan 2015) that 8 weeks of underwater treadmill training decreases walking exercise heart rate.
There is level 2 evidence (de Carvalho et al. 2006) that neuromuscular electrical stimulation gait training can increase metabolic and cardiorespiratory responses in persons with complete tetraplegia.
