Shunting
Shunting of the syrinx cavity can be performed using syringoperitoneal, syringopleural, syringosubarachnoid, or ventriculoperitoneal shunts. Most shunting procedures also involve laminectomies and duraplasties prior to the insertion of shunts (Figure 3).
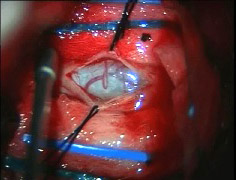
Figure 3. Drainage of syrinx followed by shunt insertion. (Elliot, NSJ 2008b)
Discussion
In all of the studies, no shunting procedure was found to be superior to another. Schaan and Jaksche (2001) in a cohort study assessed the efficacy of syringomyelia treatment in three groups of patients: Group One received various shunts only, Group Two received shunting followed by surgical creation of a pseudomeningocele, and Group Three was treated with the pseudomeningocele only. The study found improvement in sensory and motor deficits, pain and syringobulbia in all three groups. However, more patients experienced greater pain post-surgery in the shunting only group than the other two groups. It should be noted that although groups did improve on some of the outcome measures, none of the groups were significantly different from each other.
Falci et al. (1999) demonstrated that untethering and shunt tube placement among individuals without prior surgery can significantly improve light touch, pinprick and motor scores. Two case series (Lee et al. 2001; Lee et al. 2000) further examined untethering and shunting treatment in individuals with syringomyelia. In the study by Lee et al. (2001), patients were divided into three groups: untethering only, shunting only, and untethering and shunting. Improvement in motor and sensory functioning was observed in all three groups, although the groups did not significantly differ from each other. In the first group, untethering only, improvement in spasticity was more common; while the shunting only group found gait improvement to be the most common. These results are also supported by Lee et al. (2000) earlier case series which found the same outcome measures were improved by the same corresponding intervention. Furthermore, shunting alone has been reported to significantly improve pain (Hess & Foo 2001; Hida et al. 1994; Davidson, Rogers & Stoodley 2018), strength (Hess & Foo 2001), motor function (Hida et al. 1994; Davidson et al., 2018) and sensation (Hess & Foo 2001; Hida et al. 1994) in patients with syringomyelia, although, a high rate of shunt failure (36-50%) has been reported (Hess & Foo 2001; Hida et al. 1994). Another case series by Li et al. (2021) investigated the radiographic and clinical outcomes following various surgical treatments, including syrinx fenestration, adhesion lysis, and duraplasty, in 24 individuals with syringomyelia following traumatic SCI. In four of the patients, pre-existing syrinx shunts were removed, and in two others, syrinx shunts were placed. It was found that all but one patient remained clinically stable regarding motor, sensory, and bowel/bladder function post surgery. The authors noted that the only patient who experienced deterioration in motor function post surgery had undergone syringo- subarachnoid shunt placement. Due to the lack of clarity in reporting post-surgical outcomes for each type of surgical intervention, as well as the small sample size, findings should be interpreted with caution (Li et al. 2021).
One case control study (Ronen et al. 1999) reviewed charts of patients receiving either rehabilitation only or rehabilitation and shunting for syringomyelia. The study found 80% of patients in the shunting and rehabilitation group experienced functional and neurological deterioration, while patients in the rehabilitation group remained either unchanged or improved. One must be careful when drawing conclusions from such a study because allocation to either group was dictated by receiving the treatment, which presumably was given to those patients already deteriorating or those were considered at a higher risk of deterioration.
Ushewokunze et al. (2010) studied the adverse events after laminectomy and shunting and reported a reduction in syrinx size among 21 of 40 patients and a stabilization of symptoms among 27 of 40. However, symptoms deteriorated for 13 individuals including pain, increased neurological deficits, infection and CSF leakage. In 17 individuals, a second surgical procedure was required to improve deteriorating symptoms.
Only one Pre-Post Study examined the use of a myringotomy tube (Tassigny et al. 2017). Of the 17 participants in the study, only one experienced clinically worse progression of the syrinx. Additionally, between days 1-3 post-surgery 15 patients experienced shrinkage of the syrinx, with eight of those being complete (Tassigny et al. 2017).
A Pre-Post study examining just shunting (Davidson et al. 2018) found that shunting alone was enough to reduce the size of the syrinx in up to 90% of patients. Although the majority of patients improved on clinical symptoms there were no significant differences between groups for quality of life. Finally, a study by Karam et al. (2014) revealed that patients who received both shunting and duraplasty were less likely to require reoperations (3/11 patients) compared with patients who received a shunt only with 10 of 16 requiring revisions and reoperations. However, this contrast was not statistically significant. Overall, 14 patients (52%) experienced an improvement in symptoms, 10 (37%) remained stable whilst three (11%) reported a progression of symptoms without improvement. In addition, a reduction in syrinx size was reported which correlated significantly with clinical improvement as measured by Odom Score. Only one patient experienced complications post-surgery with pain and dysphagia reported; however, it was later revealed the patient had developed another syrinx larger than before. The patients received another shunt and duraplasty which resulted in improvements reported at three-month follow-up.
Conclusions
There is level 2 evidence (from one cohort, four pre-post, and five case series studies: Karam et al. 2014; Ushewokenze et al. 2010; Schaan & Jaksche 2001; Falci et al. 1999; Lee et al. 2000; Lee et al. 2001; Hess & Foo 2001; Hida et al. 1994; Tassigny et al. 2017; Davidson et al. 2018) that shunting improves pain, motor function and sensory loss in some SCI patients with syringomyelia; however, a high rate of shunt failure has been observed; these findings are tempered by level 4 evidence (from one pre-post study: Karam et al. 2014) that reported minimal clinical improvement post shunting with or without duraplasty.