Pathophysiology
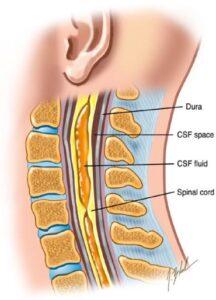
The pathophysiology of syringomyelia following SCI is not completely understood. The most supported theory is William’s “Cranial-Spinal Pressure Dissociation Theory” which involves formation of the cavity and its enlargement and extension (Williams et al. 1981). Initially, at the site of SCI, a cavity forms after liquefaction of cord tissue or hematoma (Biyani & El Masry 1994; Williams et al. 1981). The liquefaction and cyst formation at the site has been linked to microinfarcts and the release of cellular enzymes (Williams et al. 1981; Kao & Chang 1977). Cyst formation results in partial obstruction of cerebral spinal fluid movement, creating a pressure gradient between the intracranial space and spinal space (Sharma et al. 2006). The second phase, cyst enlargement and extension, is the result of this pressure gradient which has been linked to two mechanisms affecting fluid dynamics, ‘slosh’ and ‘suck’ (Biyani & El Masry 1994; Williams et al. 1981). The ‘slosh’ is due to increased epidural venous pressure and CSF movement which are triggered by everyday activities such as coughing and sneezing (Williams 1992). This pressure causes areas of structural weakness in the cord leading to proximal and distal extension of the syrinx. The second mechanism ‘suck’ is the result of a partial subarachnoid block. As the fluid is initially forced up due to increased epidural venous pressure, it returns slowly creating a pressure gradient across the partial subarachnoid block with negative pressure caudal to it (Biyani & El Masry 1994). This contributes to the syrinx formation and progression.