Mechanical Ventilation (MV) and Weaning Protocols
The indications for MV and the acute management of respiratory issues in SCI are outside the scope of this review which focuses on rehabilitation (Acute Respiratory and Mechanical Ventilation and Weaning Protocols may be found here). However, the long-term complications associated with chronic ventilator dependency need to be mentioned to highlight their importance. The overall life expectancy for people with SCI who are ventilator dependent has been increasing, especially for those who survive the first year following injury (DeVivo & Ivie 1995). Despite advances, mortality for people with ventilator dependency remains high (Shavelle et al. 2006; DeVivo & Ivie 1995).
In general, people with complete neurologic injuries at C2 and above have no diaphragmatic function and are often ventilator dependent. People with complete neurologic injuries at C3 or C4 have variable diaphragmatic function. Although they may have the potential for ventilator weaning, it is difficult to predict whether they will ultimately be successfully weaned. Research suggests that trends in improved survival observed in SCI were not seen among ventilator-dependent patients with SCI surviving the first few years post-injury, and that ventilator dependency is an independent risk factor for mortality (Shavelle et al. 2006). People with complete injuries at C5 and below typically have intact diaphragmatic function. They may require ventilatory support initially post-injury but are usually able to wean from the ventilator.
The approach to ventilator weaning in SCI remains an important and somewhat neglected issue. There is a distinct lack of controlled trials in respiratory medicine; research in this area primarily consists of retrospective reviews and small case series. The Paralyzed Veterans of America (PVA) Consortium for Spinal Cord Medicine—Respiratory management following spinal cord injury: a clinical practice guideline for health-care professionals (2005) suggests the consideration of “…progressive ventilator free breathing (PVFB) over synchronized intermittent mandatory ventilation (IMV)”. The other clinical practice guideline that we are aware of addressing SCI is the Home mechanical ventilation: A Canadian Thoracic Society clinical practice guideline. This guideline intends to provide up-to-date information and evidence-based recommendations re: preventive airway management and home ventilation with regards to a variety of conditions with respiratory consequences.
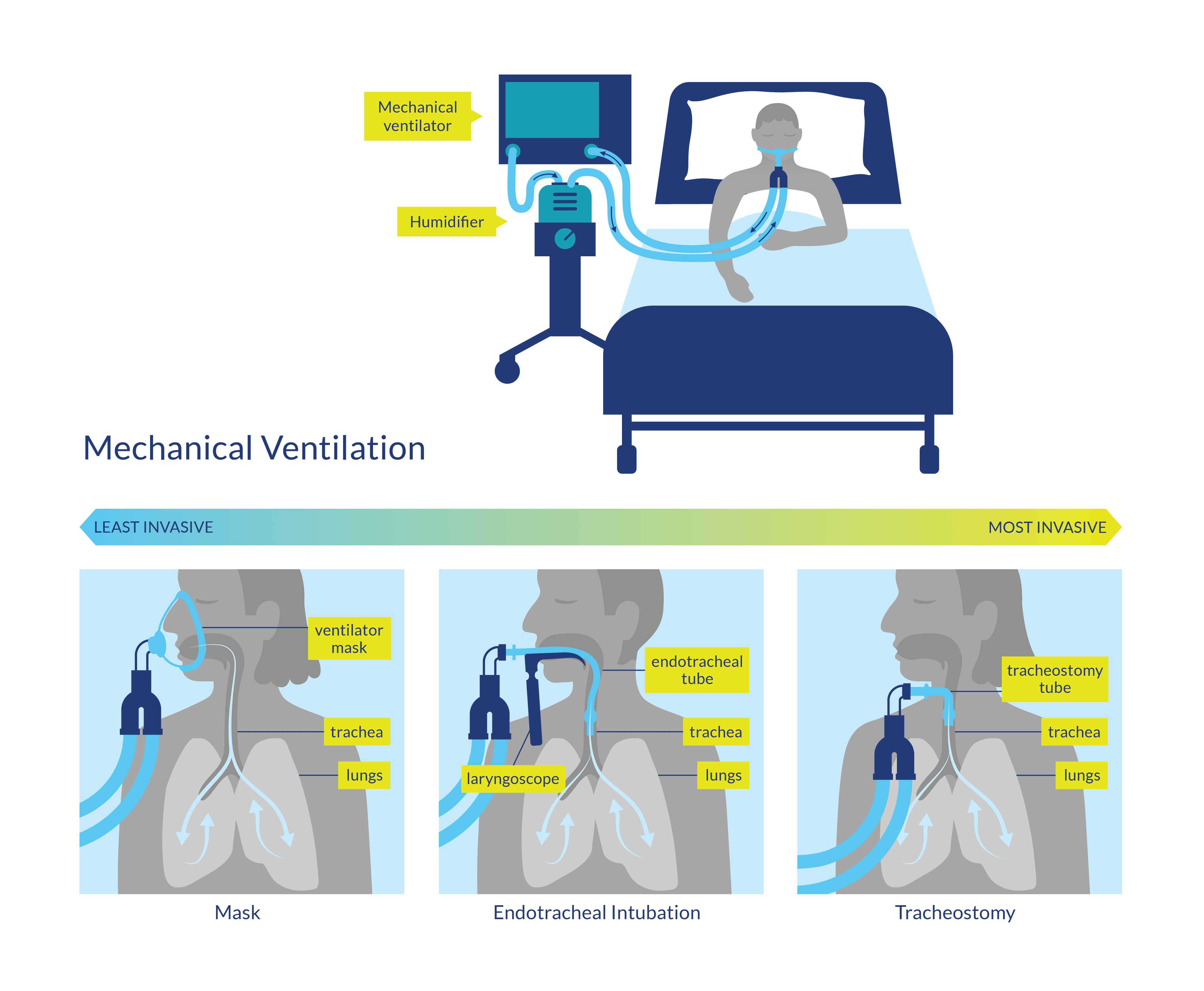
Figure 3. Mechanical Ventilation procedures
Discussion
The systematic review of Schreiber et al. (2021) included 39 studies (with 14637 patients, of which 874 were in rehabilitation units) and found that in addition to high-level lesions, multiple comorbidities, a high Injury Severity Score, elevated heart rate, and presence of TOT were also associated with increased odds of weaning failure. Furthermore, shorter time to admission to a specialized SCI center, complete lesions, presence of TOT, low VT, and high positive end-expiratory pressure were associated with a longer duration of MV (Schreiber et al. 2021). They also found that 72-82% of the patients admitted to a rehabilitative ward were either completely or partially liberated from the ventilator, 35.5% (11.3 – 70.5%) developed pneumonia, and less than 1% (0 – 18.5%) died (Schreiber et al. 2021).
Peterson et al. (1994) retrospectively compared weaning methods in people with C3-C4 SCI. Overall 83% of participants were successfully weaned with PVFB (also known as T-piece weaning) being the most successful technique.
Gutierrez et al. (2003) developed an evidence based resistive and endurance protocol to improve ventilatory muscle strength and endurance in people with ventilator-dependent cervical SCI. The protocol included 4 daily phases with rests between each phase: pre-training optimization (Trendelenburg positioning, trachea suctioning, bronchodilator use, and lung hyperinflation); inspiratory/expiratory resistive training; on-ventilator endurance training; and off-ventilator endurance training. Although the pilot study only included 7 participants, it showed promising results with respect to increasing inspiratory pressure, expiratory pressure and VC, and ultimately ventilator weaning, especially in people with low tetraplegia (C4-C7) (Gutierrez et al. 2003).
Onders et al. (2010) evaluated diaphragm pacing (DP) as a weaning method in 20 participants who also had cardiac pacemakers and found no immediate or long-term device-to-device interactions. All patients could go >4 hours without mechanical ventilators, and 71% could go 24 hours continuously with DP.
Wong et al. (2012) retrospectively analyzed the charts of 24 people with high cervical SCI (C1-C4) who underwent high tidal volume ventilation (HVtV) treatment, high frequency percussive ventilation (HFPV) treatment and/or and mechanical insufflation-exsufflation (MIE) treatment in a specialized SCI treatment unit. All patients showed improvements in their respiratory status and 14 patients were successfully weaned from their ventilators.
Gundogdu et al. (2017) retrospectively analyzed 35 participants with cervical SCI with MV and/or TOT tube for a prolonged period. MV-dependent patients who underwent respiratory rehabilitation, MV weaning, and a TT decannulation program, showed an improvement in some respiratory parameters (MIP, MEP and peak cough flow [PCF]) and a rate of 70% of successful weaning from MV and TT, while tracheostomized patients who underwent respiratory rehabilitation and a TT decannulation program showed an increase in PCF and a rate of 92% of successful on decannulation. The mean duration of weaning from MV and TT decannulation was 37.0 ± 11.6 and 31.7 ± 16.9 days, respectively.
Kaufman et al. (2022) prospectively studied a treatment protocol using a surgical algorithm involving DP, phrenic nerve reconstruction, and diaphragm muscle replacement. They analyzed 10 patients with ventilator-dependent cervical tetraplegia and ASIA A, who received different treatments based on the extent of neuromuscular dysfunction (pacemaker alone, pacemaker + phrenic nerve reconstruction or pacemaker + diaphragm muscle replacement), showing 4 patients who achieved a partial and 4 a complete weaning.
Toki et al. (2021) retrospectively analyzed 14 patients with TOT, SCI, and ASIA A who received a protocol of non-invasive ventilation (NIV) which assessed ventilator setting, interface, and respiratory training. 11 patients were switched to NIV, showing that a history of TOT ventilation of less than one year was correlated with successful switching (100%), compared with TOT ventilation of ≥ 1 year.
Prospective studies on weaning protocols are required to determine the best way to assess, treat and wean people requiring MV following SCI.
 Mechanical insufflation-exsufflation (e.g., using a “Cough Assist machine”) is a therapy in which the device gradually inflates the lungs (insufflation), followed by an immediate and abrupt change to negative pressure, which produces a rapid exhalation (exsufflation), which simulates a cough, and helps to clear secretions.
Mechanical insufflation-exsufflation (e.g., using a “Cough Assist machine”) is a therapy in which the device gradually inflates the lungs (insufflation), followed by an immediate and abrupt change to negative pressure, which produces a rapid exhalation (exsufflation), which simulates a cough, and helps to clear secretions.
Conclusion
There is level 4 evidence (from one case series Wong et al. 2012) that the implementation of specialized respiratory management (HVtV, HFPV, MIE) resulted in an improvement of respiratory status in all study participants.
There is level 3 evidence (from one retrospective study: Gundogdu et al. 2017) that the implementation of a respiratory rehabilitation protocol, consisting of respiratory assessment and management of different aspects, improved respiratory parameters of MV-dependent patients before/after the weaning protocol and also in tracheostomized participants; provided a rate of 70% of successful weaning from MV ant TT in MV-dependent patients, a rate of 96% of TOT closure and a rate of 85.7% of decannulation in patients with cervical SCI.
There is level 4 evidence (from one prospective study: Kaufman et al. 2022) that the implementation of a treatment protocol which included a surgical algorithm that involved DP, phrenic nerve reconstruction, and diaphragm muscle replacement provided a rate of 80% of successful weaning (40% partial weaning and 80% complete weaning) in patients with ventilator-dependent cervical tetraplegia and ASIA A.
There is level 4 evidence (from one retrospective study: Toki et al. 2021) that the implementation of a protocol of NIV which assess ventilator setting, interface, and respiratory training in 5 steps provided a rate of 78.6% of a successful switch to NIV in patients with SCI and ASIA A.
There is level 4 evidence (from one case series study: Peterson et al. 1994) that PFVB protocol is more successful for weaning people with C3 and C4 spinal cord injuries than IMV.
There is level 4 evidence (from one case series study: Onders et al. 2010) that DP served as an effective weaning protocol in all participants.
There is level 4 evidence (from one pre-post study: Gutierrez et al. 2003) that a resistive and endurance protocol increases inspiratory pressure, expiratory pressure, and VC especially in low tetraplegia (C4-C7).
There is level 4 evidence (from one retrospective case series: Romero-Ganuza et al. 2015) that though many people with SCI will require MV they can be successfully weaned from it.
