Clinical Focus: Multidisciplinary Approach to Sexual and Fertility Rehabilitation
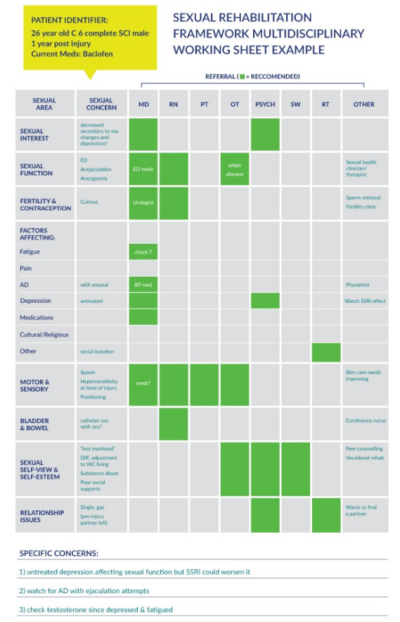
Many studies have identified improvement in sexual function as a priority for persons with SCI. Due to the various secondary sensory, motor, and autonomic consequences following SCI and due to the complexity of sexuality per se, this area can be overwhelming to many health care professionals. The literature indicate that sexual and fertility rehabilitation must be addressed in a biopsychosocial manner and include various disciplines. The Sexual Rehabilitation Framework (SRF) is a user-friendly and simplified way to proactively address the major biopsychosocial areas of sexuality and to create a plan of action for the person with SCI. It is an adjunct tool to the full sexual history, and it encourages all disciplines involved in SCI rehabilitation to address the issue of sexual function in the same manner as they would other activities of daily living.
Eight areas included in the SRF are:
- Sexual drive/interest,
- Sexual functioning,
- Fertility and contraception,
- Factors associated with the condition,
- Motor and sensory influences,
- Bladder and bowel influences,
- Sexual self-view and self-esteem, and
- Partnership issues.
The use of the SRF is encouraged in both inpatient and outpatient settings. Multidisciplinary or interdisciplinary team work is encouraged in sexual and fertility rehabilitation to move clinicians toward providing proactive and comprehensive care for individuals with SCI or other chronic disabilities. To assess and manage sexual issues, single or multiple disciplines can be recruited to suit the needs each individual client. Health care providers can include physicians, nurses, occupational therapists, physiotherapists, recreational therapists, psychologists, and social workers. Peer experience around sexuality can also be invaluable, but will depend on the availability of peer programs or counselors. In its simplest form, the SRF can be a checklist that covers the sexual areas and notes how one area can affect another area. The SRF is contextualized within the 3 principles of sexual rehabilitation16:
- Maximize the remaining capacities of the total body before relying on medications or aids (learning new body maps, breathing, visualization methods, mindfulness exercises),
- Adapt to residual limitations by utilizing specialized therapies (use of vibrators, mobility devices, training aids, phosphodiesterase type 5 inhibitors, vacuum device aids), and
- Stay open to rehabilitative efforts and new forms of sexual stimulation, with a positive and optimistic outlook.
For an example of what a variety of professionals would be responsible for in a multidisciplinary approach, refer to figure below.
Sexual Health Clinicians/Sex Therapists (SHC/ST): The role of sexual health clinicians (usually nurses) specially trained in sexuality and chronic illness/disability and those of community sexual therapists (often psychologists) goes beyond providing permission to discuss the area of sexuality and normalizing and validating client’s concerns. SHC/STs are trained to take full sexual histories and to provide more specific information related to a client’s particular concern. With or without other disciplines, they can intervene with therapeutic options (i.e., looking at erection enhancement options, fertility procedures, and techniques to address anejaculation and/or premature ejaculation, ways to experience pleasure in the context of limited or decreased sensation, mindfulness work). Specialized training and knowledge in sexuality and disability are required in this role.
Occupational therapists (OTs): OTs are in an excellent position to normalize sexual health as part of rehabilitation and assist in specifics for sexual activity, such as adaptive sexual devices, environmental controls, and adapted clothing.
Physiotherapists (PTs): A PT is often the first clinician that clients see in community, and he or she can be very effective in opening the conversation, normalizing sexual health rehabilitation as part of overall rehabilitation, and connecting individuals to necessary supports.
Psychologists and counselors: Depression, anxiety, loss and grief, role changes, and relationship discord are common post SCI and can have a significant effect on sexual health (sexual drive, relationships, etc).
Social Workers (SW): In the context of sexual rehabilitation, the SW is able to work with the client or group to seek out individual resources as well as sources of support and resources in the community to support clients to attain their goals for their sexual health/relationships.
Recreational therapists (RTs): An RT could teach a client new or adaptive ways of expressing themselves through activities such as sports, art, exercise, and dance. This could affect a person’s sense of his or her sexual self in the world and how he or she is seen as a sexual person by others.
Vocational Rehabilitation Therapists: Loss of employment following an injury can be devastating to a person’s sense of self. As a result, confidence and self-esteem, including sexual self-esteem, can be negatively impacted. Supporting a person to return to previous employment, train for a new occupation, or assume a volunteer role is important for re-establishing a sense of purpose, accomplishment, and wholeness to a person’s life.
