Sleep Disordered Breathing in SCI
SDB, commonly known as sleep apnea, is a disease characterized by recurrent collapse of the upper airway during sleep leading to nocturnal hypoxemia and sleep fragmentation. Characteristic symptoms include loud snoring, excessive daytime sleepiness, and nocturnal choking. Risk factors for disease include alcohol use, sedatives, obesity, increased age, and male gender. Because of activation of systemic inflammation and the sympathetic nervous system, sleep apnea may be an independent risk factor for the development of cardiovascular disease. In the able-bodied, sleep apnea is relatively common and under-diagnosed.
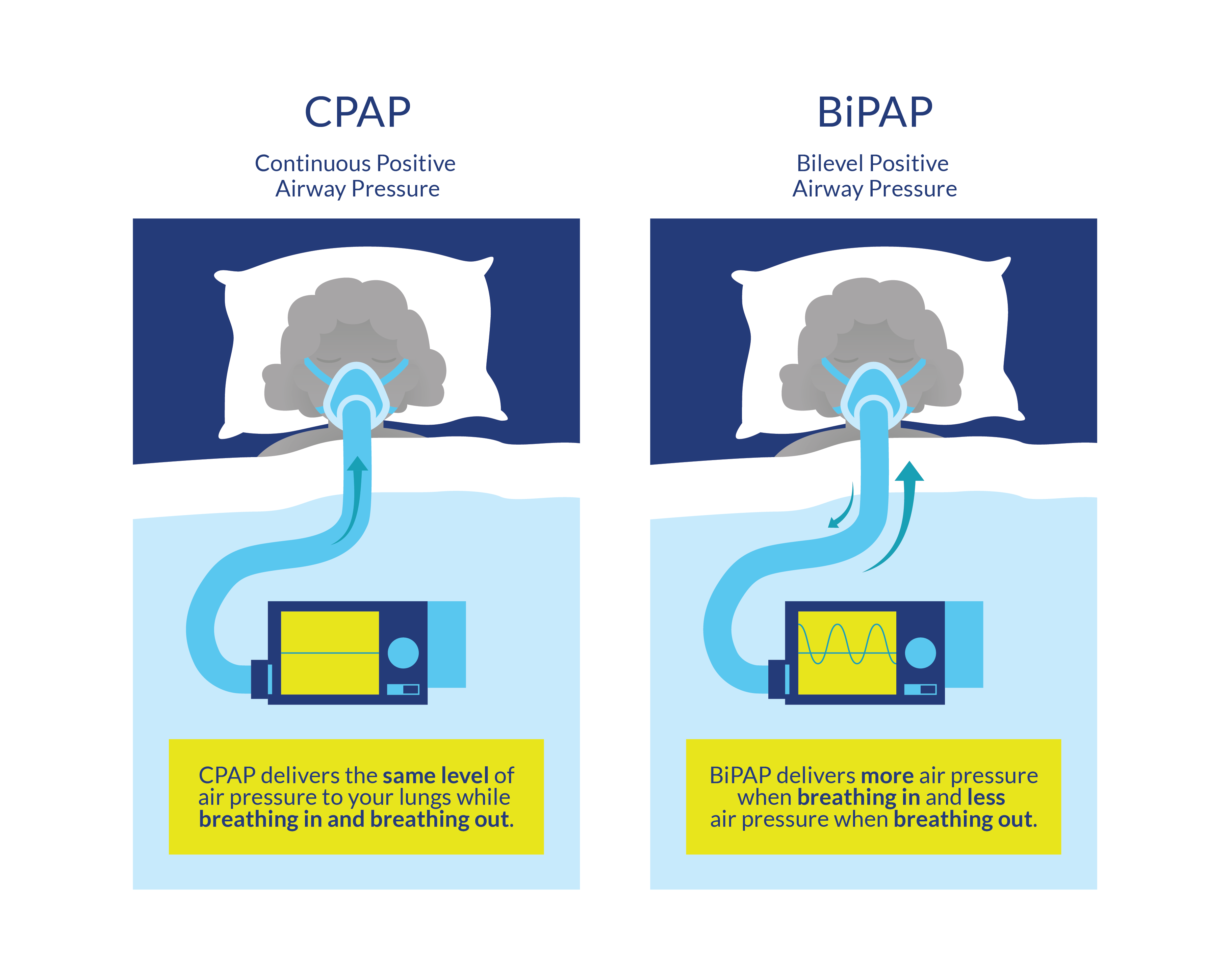
Generally, the first line treatment of sleep apnea is lifestyle counseling (i.e., weight loss, avoidance of alcohol). There are different types of sleep apnea and they require different treatment approaches; obstructive sleep apnea (OSA) occurs when throat muscles relax, and central sleep apnea occurs when your brain does not send proper signals to the muscles that control breathing. OSA can be treated with continuous positive airway pressure (CPAP) therapy, considered to be first-line therapy. This consists of a mask placed on the face attached to an air compressor via plastic tubing. CPAP devices establish a positive pressure in the upper airway preventing its collapse during sleep. Studies of CPAP in people without SCI demonstrate significant benefits in terms of reducing sleepiness and preventing motor vehicle crashes. Other therapies that have been used to treat OSA include mandibular advancement devices (dental splints) and upper airway surgery. Central sleep apnea requires a back-up rate, and sleep-related hypoventilation and a pressure differential between inspiration and expiration (a treatment called Bi-level PAP) (Chiodo et al. 2016). Research shows that central apnea is more common in patients with tetraplegia than in patients with paraplegia (Chiodo et al. 2016).