Body-Weight Supported Treadmill Training (BWSTT)
Body-weight supported treadmill training (BWSTT) is an exercise protocol that involves supporting an individual over the top of a motorized treadmill with a counterbalanced harness system. The premise of all BWSTT protocols is to offset some of an individual’s body weight to reduce the work associated with upright walking, using a weight stack to adjust the magnitude of support and treadmill speed to adjust the intensity of exercise. The degree of support, as well as the amount of progression across a training period, is highly individualized, determined by a trained therapist observing proper gait and cardiovascular responses. While BWSTT has garnered attention in functional movement rehabilitation, previous studies have indicated this strategy can also target conventional outcomes of cardiorespiratory fitness through a lower-intensity aerobic challenge. While the resources for this modality are high (i.e., specialized treadmill, lead therapist, volunteers to assist with leg movements), there is potential for BWSTT to target multiple exercise domains including upright posture challenges, cardiovascular effort, and lower-limb skeletal muscle involvement.
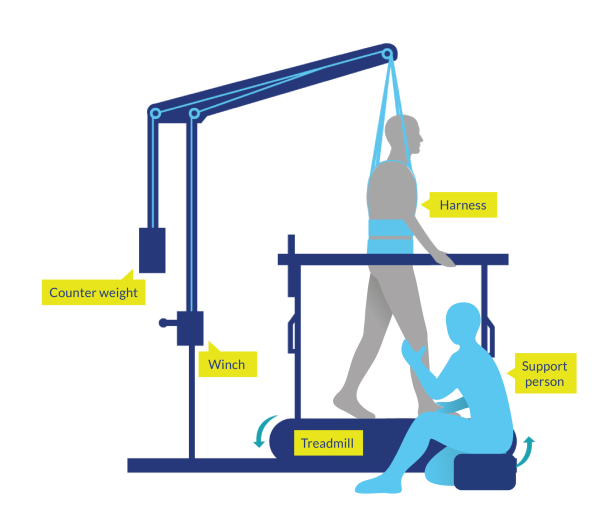
Figure 2. Body-Weight Supported Treadmill Training (BWSTT)
Discussion
Seven BWSTT studies examined individuals with incomplete SCI, who engaged in active walking supported either above ground or above treadmills with individually-determined body weight support. In general, there were small increases in cardiorespiratory fitness and improvements in submaximal heart rate, indicating a small degree of cardiovascular changes after 4-13 weeks of BWSTT.
Two RCT studies were completed for high-level evidence. Alexeeva et al. (2011) used an RCT design to evaluate two forms of body-weight supported walking (i.e., fixed track vs. treadmill) vs conventional physical therapy and observed small, but clinically meaningful improvements in VO2peak. However, as these results were not statistically significant, some caution should be taken in their interpretation. Millar et al. (2009) conducted a 4-week RCT with a cross-over design, but did not observe any improvements in heart rate variability, a marker of autonomic nervous system function. They did indicate improvements in heart rate complexity, another marker of autonomic function. Changes in nervous system function were also noted by Ditor et al. (2005), who indicated improvements in heart rate variability after 6 months of BWSTT.
There is good evidence to indicate improved respiratory function after BWSTT in individuals with incomplete SCI. Both Terson de Paleville et al. (2013) (12-week BWSTT) and Soyupek et al. (2009) (6-week BWSTT) demonstrated improvements in forced vital capacity after training, which measures the total amount of air exhaled during a maximal breathing effort. Both studies were pre-post designs with small sample sizes, but provide corroborating findings for respiratory improvements after BWSTT.
Three studies examined individuals with motor complete SCI, using completely passive gait training in the upright position. Ditor et al. (2005) did not observe improvements in cardiorespiratory fitness, although there were small effects on markers of lower-limb vascular health. de Carvalho & Cliquet (2005) indicated increased blood pressure control after 3 months of BWSTT, while de Carvalho et al. (2006) indicated improved submaximal exercise capacity after 6 months of passive BWSTT, as noted by an increase in exercise oxygen consumption (VO2), ventilation and exercise blood pressure.
Five studies used robotic-assisted body-weight supported treadmill training (RABWSTT), with active initiation of gait. Gorman et al. (2019) used a RCT design to evaluate the efficacy of robotic (exoskeleton) therapy or aquatic therapy to increase cardiorespiratory fitness. Exoskeleton training was not able to increase VO2peak during conventional maximum arm ergometry testing but was able to increase mode-specific VO2 during exoskeleton walking sessions. Similarly, Gorman et al. (2016) demonstrated an increase in VO2 during RABWSTT-specific training. Hoekstra et al. (2013) used a 24-session pre-post design to evaluate fitness in individuals with incomplete SCI. No differences were observed in submaximal VO2 post-intervention, though improvements in submaximal heart rate and resting heart rate were observed. While Turiel et al. (2011) indicated improvements in diastolic heart function after 6 weeks of RABWSTT, they did not report translations into improved cardiorespiratory fitness. Finally, in the only positive study, Cheung et al. (2019) used an RCT design to indicate improvements in cardiorespiratory fitness after 8 weeks of RABWSTT; however, the magnitude of improvement was so small it would be considered negligible in a functional capacity.
Conclusions
There is Level 1b evidence (Millar et al. 2009) that at least 1 month of 3x/week BWSTT can improve autonomic nervous system function.
There is Level 4 evidence (Jack et al. 2009) that 16 weeks of 3x/week BWSTT can improve VO2peak.
There is Level 4 evidence (Stevens et al. 2015) that 8 weeks of 3x/week BWSTT can improve submaximal exercise capacity.
There is Level 4 evidence (Soyupek et al. 2009; Terson de Paleville et al. 2013) that 6 weeks of 5x/week BWSTT can improve respiratory function.
There is Level 4 evidence (de Carvalho & Cliquet 2005; de Carvalho et al. 2006; Ditor et al. 2005) that at least 3 months of passive BWSTT can improve aspects of cardiovascular function in individuals with motor-complete injuries.
