Repetitive Transcranial Magnetic Stimulation (rTMS) and Paired Corticospinal-Motoneuronal Stimulation (PCMS)
Repetitive transcranial magnetic stimulation (rTMS) has been widely explored as a tool for treating a variety of disorders, including depression (Martin et al. 2003; Couturier et al. 2005), pain (Lima & Fregni 2008), and motor disorders following Parkinson’s disease (Elahi et al. 2009) and stroke (Corti et al. 2011). Experimental studies in humans have shown that low-frequency rTMS (<1 Hz) can reduce the excitability of the motor cortex whereas high-frequency rTMS (>1 Hz) causes an increase in motor cortical excitability (Kobayashi & Pascual-Leone 2003). Given the ability for rTMS to modulate cortical excitability, there has been much interest in exploring its potential to facilitate supraspinal connectivity as a means to promote motor recovery and function. The recovery of functional ambulation, following motor-incomplete SCI, has been shown to be associated with enhanced excitability of motor cortical areas (Winchester et al. 2005) and corticospinal connectivity to the lower limb (Thomas & Gorassini 2005).
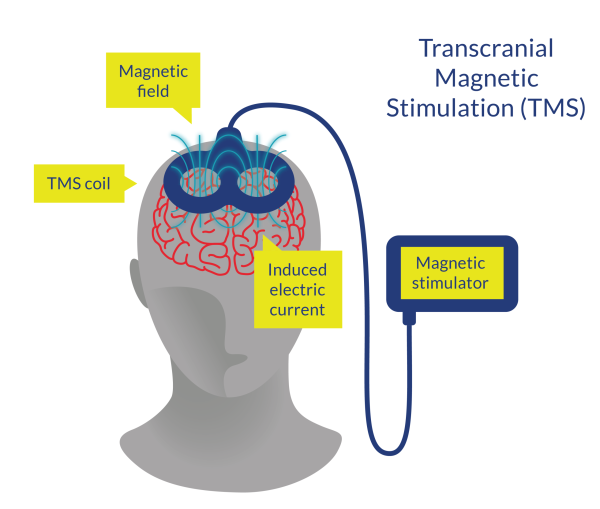
Figure 9. Transcranial Magnetic Stimulation (TMS)
Discussion
Few studies have investigated the effects of rTMS on walking-related outcomes in patients with acute, subacute, or chronic SCI (Benito et al. 2012; Deng et al. 2024; Krogh et al. 2022; Kumru et al. 2016a; Naro et al. 2022; Nogueira et al. 2024). Two RCTs found the same results; participants who had rTMS plus usual care improved significantly more than those who had sham rTMS and usual care on LEMS, but both groups improved on the 6MWT and 10MWT without statistical differences (Krogh et al. 2022; Kumru et al. 2016a). Benito et al. (2012) found similar results; all participants completed OGT and improved post-training in step length and TUG, but only the participants receiving rTMS improved post-training in LEMS and spasticity reduction.
Lastly, the RCT by Deng et al. (2024) compared real and sham intermittent theta burst stimulation (iTBS) (which is a mode of TMS) dual-target stimulation applied before conventional physical therapy in patients with incomplete and acute SCI. After 21 days of treatment, it was shown that there were statistically significant (P < 0.05) differences between groups, favoring the iTBS group, in the muscle strength of the knee flexors and knee extensors, LEMS, SCIM, step length and step frequency, and in the ground reaction force.
On the other hand, in patients with incomplete and chronic SCI, the RCT by Nogueira et al. (2024) compared a rTMS protocol followed by BWSTT (with visual feedback on the real-time stride length, provided through a mirror to maintain step symmetry and control postural compensation) for 12 sessions with the same intervention but with a sham rTMS application. After the 12th session, there was no difference between groups in walking independence (WISCI II) (Nogueira et al. 2024). Additionally, compared to baseline, LEMS and SCIM-III mobility scores were increased after 12 sessions in the BWSTT/rTMS real group but not in the sham group (Nogueira et al. 2024). The authors also showed that WISCI II scores after the 6th session were higher in the BWSTT/rTMS real than in the sham group; suggesting that combining BWSTT with rTMS could lead to earlier gait improvement in patients with chronic incomplete SCI.
It should be noted that rTMS seems to be safe; however, there were some side effects during the trials. Krogh et al. (2022) reported that one patient in the real stimulation group dropped out due to a seizure during stimulation, and two participants in the sham stimulation group reported mild and transitory headaches following their first treatment session. Kumru et al. (2016a) and Benito et al. (2012) stated that all participants tolerated the interventions, with the participants in real rTMS reported only mild undesired effects (slightly uncomfortable twitching of facial muscles or difficulty to speak because of facial muscle contraction during real rTMS [n = 8 and n = 6, respectively], and mild headache one hour after the first rTMS session [n = 1 and n = 0, respectively]).
Conclusions
There is level 1 evidence (from 2 RCTs: Krogh et al. 2022; Kumru et al. 2016a) that the application of rTMS immediately before lower limb training sessions or BWSTT with Lokomat provides significant improvements in LEMS, but similar improvements in walking-related outcomes (6MWT and 10MWT) compared with the same intervention but with a sham rTMS application in participants with motor-incomplete and acute SCI.
There is level 1 evidence (from 1 RCT: Benito et al. 2012) that rTMS before overground LT provides significant improvements in lower limb strength (LEMS) and walking speed (10MWT) in patients with motor-incomplete SCI.
There is level 1 evidence (from 1 RCT: Deng et al. 2024) that iTBS (a mode of TMS) dual-target stimulation applied before conventional physical therapy for 21 days provides higher and significant improvements in the muscle strength of the knee flexors and knee extensors, LEMS, SCIM, step length and step frequency, and in the ground reaction force; compared with a sham iTBS intervention plus conventional physical therapy; in participants with incomplete and acute SCI.
There is level 1 evidence (from 1 RCT: Nogueira et al. 2024) that an rTMS protocol followed by BWSTT for 12 sessions provides significant improvements in LEMS and SCIM-III, but not in WISCI II, compared with a sham rTMS application followed by BWSTT in patients with incomplete and chronic SCI.
