Robot-Aided Gait Training with End-Effector Devices
In recent years, various types of robotic devices have been developed for motor rehabilitation (Choi et al. 2019). Generally, these robotic devices are divided into two categories based on the driving principle: exoskeleton and end-effector type robots (Choi et al. 2019). Exoskeleton robots move in parallel to the skeleton of the patient, so that no additional degrees-of-freedom or ROM are needed and each single joint is guided along a preprogrammed trajectory (Venenan et al. 2007; Molteni et al. 2019). End-effector type robots place patient’s feet on footplates, generating movements from the most distal segment of the extremity in trajectories that simulate the stance and swing phases of walking (Hesse et al. 2010; Molteni et al. 2019).
Discussion
Overall, end-effectors seemingly allow achievement of greater gait recovery as compared to grounded exoskeletons in stroke populations (Mehrholz & Pohl 2012; Schröder et al. 2019); however, there are fewer studies in SCI populations. Specifically, there are two studies which assessed the effects of walking training with an end-effector device in walking and lower limb strength outcomes in patients with acute SCI. The RCT by Shin et al. (2023) included 29 participants with incomplete (AIS C-D) and acute SCI. Participants in the intervention group performed RAGT with an end-effector device for four weeks, five times per week, 30 minutes each session (Shin et al. 2023). Additionally, participants performed conventional training, which consisted of 30 minutes of ergometer training and 30 minutes of sitting and standing balance training, sit-to-stand training, OGT if possible, and strengthening exercises (Shin et al. 2023). Participants assigned to the control group received the same conventional training with same dosage (30 minutes of ergometer and 1 h of the rest of the training) (Shin et al. 2023). After four weeks of training both groups showed significant improvements in walking endurance (6MWT), walking speed (10MWT), walking ability (WISCI II), lower limb strength (LEMS), balance (BBS), and functional independence (SCIM-III mobility subscore); however, walking ability significantly improved more in the RAGT group than in the control group (Shin et al. 2023).
In a prospective controlled trial, Shin et al. (2021) assessed if 30 min of RAGT with the end-effector device plus one hour of conventional physiotherapy, five times per week, had effects on walking outcomes in 13 patients with acute tetraplegia (n = 11) or paraplegia (n = 2) (mean time since injury 48 [19-139] days). After four weeks of intervention, gait speed (10MWT), gait endurance (6MWT), muscle strength (LEMS) and walking ability (WISCI II) showed significant improvements; and one patient with paraplegia AIS C improved to AIS D (Shin et al. 2021). They also did a stratified analysis dividing groups by their proprioception levels of the knee and ankle; the participants who had at least grade 2 proprioceptive abilities in their knees and ankles improved significantly more in functional walking than those without (p= 0.037).
Lastly, the pre-post study (feasibility) by Choi et al. (2019) assessed patients with different neurologic disorders, including SCI (n = 40, AIS C-D). After 24 sessions of RAGT (30 min, five times per week, for four weeks) the subgroup of participants with SCI showed significant improvements in lower extremity strength (Medical Research Council scale) and ambulation ability (functional ambulation category [FAC]) (Choi et al. 2019). Although no serious adverse events occurred during sessions; 11.6% of the total sample failed to complete the RAGT (Choi et al. 2019). The reasons included decreased cooperation, musculoskeletal pain, saddle seat discomfort, excessive body-weight support, joint spasticity or restricted joint motion, urinary incontinence from an indwelling urinary catheter, and fatigue (Choi et al. 2019). These three studies used the end-effector device called Morning WalkÒ for RAGT, which is an end-effector type robot and the first gait training robot using a saddle for weight support (Shin et al. 2021) (Figure 2).
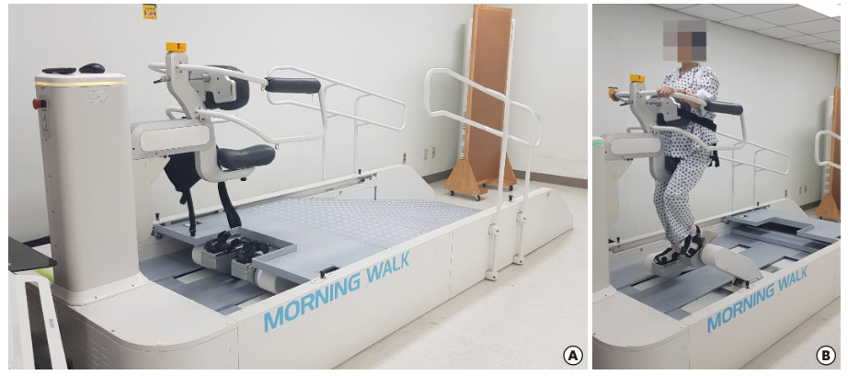
Figure 2. The Morning Walk device. From (Choi et al. 2019). Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0).
To date, the pre-post study of Calabrò et al. (2021) was the only study where patients with SCI were provided with RAGT by means of the G-EO System device, which is a (non-treadmill) end-effector device made of two footplates with three degrees of freedom on which the harness secured the patient’s stand (Calabrò et al. 2021) (Figure 3). Fifteen patients with subacute and incomplete SCI continued all other rehab activities regularly and were provided with a daily session of the end-effector G-EO System device, six days per week, for two months (Calabrò et al. 2021). It was found that patients achieved a clinically significant improvement in gait velocity (10MWT), sensory and motor functions of ASIA scale, disability burden (SCIM-III), functional ambulation (WISCI II), and quality of life (SF-36) up to six months post-treatment (Calabrò et al. 2021).
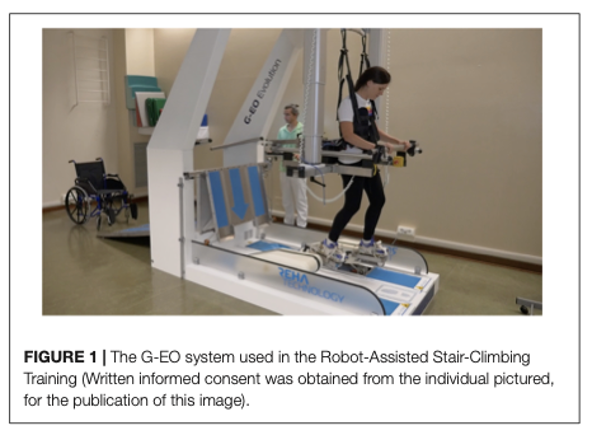
Figure 3. The G-EO System device. From (Gandolfi et al. 2019). Creative Commons Attribution License (CC BY).
Conclusions
There is level 2 evidence (from 1 RCT: Shin et al. 2023) that RAGT with an end-effector device (Morning WalkÒ) plus conventional physical therapy performed five times per week for four weeks provides significantly higher improvements in walking ability (WISCI II) than conventional physical therapy alone for people with acute and incomplete SCI.
There is level 2 evidence (from 1 prospective controlled trial: Shin et al. 2021) that RAGT (with Morning WalkÒ) with visual feedback and conventional physiotherapy provides improvements in gait speed (10MWT), gait endurance (6MWT), muscle strength (LEMS) and walking ability (WISCI II) in patients with acute (mean time since injury 48 days) motor incomplete SCI. The participants with higher proprioceptive abilities in their knees and ankles improved significantly more in functional walking than those without.
There is level 4 evidence (from 1 pre-post study: Choi et al. 2019) that RAGT (with Morning WalkÒ), performed five times a week, for a total of 24 sessions, provides significant improvements in a subgroup of participants (n = 40) with incomplete SCI.
There is level 4 evidence (from 1 pre-post study: Calabrò et al. 2021) that a 2-month program of daily sessions of RAGT with the end-effector device using the G-EO System, added to all other regular rehab activities, provides a significant improvement in motor AIS, gait velocity (10MWT) and walking ability (WISCI II) at the end of the intervention, and these improvements are retained up to six months of follow-up in patients with incomplete and subacute SCI.
