Repetitive Transcranial Magnetic Stimulation (rTMS) and Other Approaches for Standing Balance
Repetitive transcranial magnetic stimulation (rTMS) has been widely explored as a tool for treating a variety of disorders, including depression (Martin et al. 2003; Couturier et al. 2005), pain (Lima & Fregni 2008), or motor disorders following Parkinson’s disease (Elahi et al. 2009) and stroke (Corti et al. 2011). Experimental studies in humans have shown that low-frequency rTMS (<1 Hz) can reduce the excitability of the motor cortex whereas high-frequency rTMS (>1 Hz) causes an increase in motor cortical excitability (Kobayashi & Pascual-Leone 2003). Given the ability for rTMS to modulate cortical excitability, there has been much interest in exploring its potential to facilitate supraspinal connectivity or restore the balance of interhemispheric inhibition (in stroke) as a means to promote motor recovery and function. The recovery of functional ambulation following motor-incomplete SCI has been shown to be associated with enhanced excitability of motor cortical areas (Winchester et al. 2005) and corticospinal connectivity to the lower limb (Thomas & Gorassini 2005).
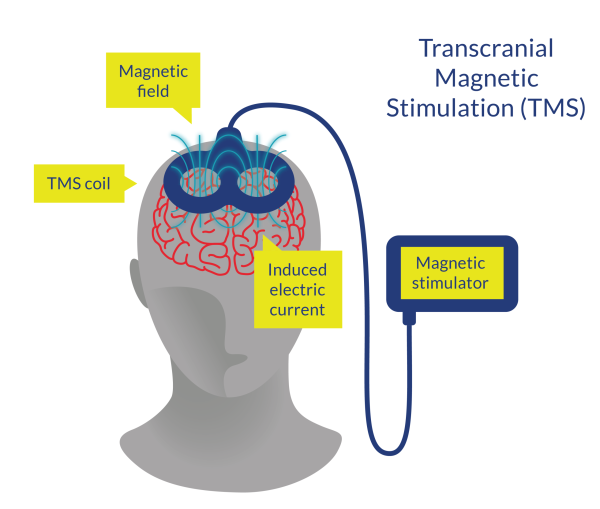
Figure 5. Transcranial Magnetic Stimulation (TMS)
Recently, other related neuromodulation approaches have been developed, such as the non-invasive brain stimulation (rTMS and simultaneous transvertebral direct current stimulation [tvDCS]) (Naro et al. 2022).
Discussion
Few studies have investigated the effects of rTMS on gait, balance, and strength outcomes in patients with acute or subacute SCI (Benito et al. 2012; Krogh et al. 2021; Naro et al. 2022). Krogh et al. (2021) compared 22 min of active or sham application of rTMS immediately before training sessions, which consisted of lower limb resistance training (twice a week) and lower limb physical therapy (thrice a week) in 20 participants with motor-incomplete and acute SCI. After 4 weeks of training, LEMS improved significantly more in the active group; meanwhile, both groups improved in the TUG test, 6MWT and 10MWT (Krogh et al. 2021). Benito et al. (2012) showed that after 15 consecutive rTMS sessions applied before overground gait training in patients with subacute and motor incomplete SCI there were significant improvements in LEMS and 10MWT in the rTMS group, though both groups showed similar improvements in standing balance (TUG).
It should be noted that rTMS seems to be safe; however, there were some side effects during the trials. Krogh et al. (2021) reported that one patient in the real stimulation group dropped out due to a seizure during stimulation and two participants in the sham stimulation group reported mild and transitory headaches following their first treatment session. Benito et al. (2012) stated that all participants tolerated the intervention, with the participants in real rTMS reporting only mild undesired effects (slightly uncomfortable twitching of facial muscles during real rTMS [n=6]).
The case control of Naro et al. (2022) was the first study assessing both rTMS and tvDCS (namely non-invasive brain stimulation [NIBS]) with robot-aided rehabilitation. Forty participants with incomplete thoracic SCI were retrospectively divided based on whether they received a daily NIBS intervention before BWSTT or only BWSTT (Naro et al. 2022). After 8 weeks of training and at 3 months follow-up assessment, both groups improved in gait-related (10MWT, 6MWT, WISCI II and FIM-L), strength-related (LEMS), balance-related (TUG), and spasticity-related (Modified Ashworth Score) outcomes; but walking speed, FIM-L, strength and walking ability were found to have more significant increases following robot-assisted rehabilitation + NIBS compared to robot-assisted rehabilitation alone (Naro et al. 2022). However, this combined approach and its promising data need to be confirmed with more extensive RCTs incorporating objective clinical and neurophysiological measures of corticospinal and spinal excitability.
Conclusions
There is level 1 evidence (from 1 RCT: Krogh et al. 2021) that the application of rTMS immediately before lower limb training sessions provides significant improvements in LEMS, but similar improvements in walking-related outcomes (TUG test, 6MWT and 10MWT) compared with the same intervention but with a sham rTMS application in participants with motor-incomplete and acute SCI.
There is level 1 evidence (from 1 RCT: Benito et al. 2012) that rTMS before overground locomotor training provides significant improvements in lower limb strength (LEMS) and walking speed (10MWT); however, may not afford further benefits in dynamic balance (TUG) over overground locomotor training alone (with sham stimulation) in patients with motor-incomplete and subacute SCI.
There is level 3 evidence (from 1 case control study: Naro et al. 2022) that the addition of rTMS plus tvDCS to BWSTT with Lokomat provides significantly more improvements in walking speed (10MWT), FIM-L, strength (LEMS) and walking ability (WISCI II) in comparison with BWSTT alone, but not in walking endurance (6MWT) and balance (TUG) in patients with incomplete and subacute SCI with spasticity.
