Repetitive Transcranial Magnetic Stimulation
After a lesion, functional reorganization of the remaining circuits at the cortical and subcortical levels can contribute to the recovery of function. Repetitive transcranial magnetic stimulation (rTMS) s a non-invasive technique that has been shown to modulate cortical excitability and induce changes over the descending corticospinal output (Kumru et al. 2010). This cortical modulation may be useful in promoting active recovery of motor function to obtain functional benefit from gait rehabilitation. Previous studies have shown rTMS to be beneficial in reduced spasticity among patient with multiple sclerosis, cerebral palsy, and spastic quadriplegia (Wassermann & Lisanby 2001).
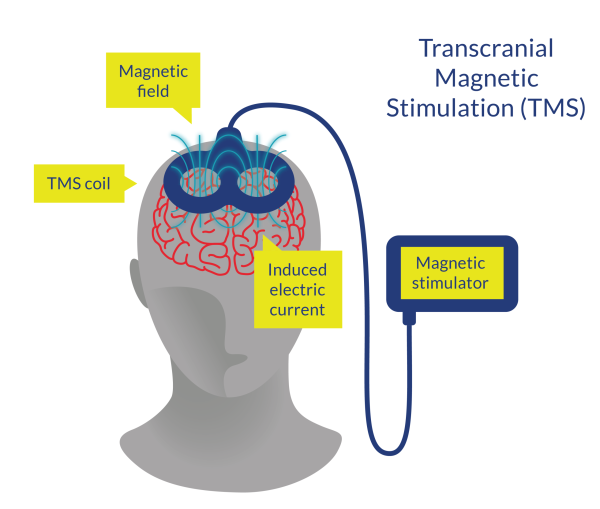
Figure 1. Transcranial Magnetic Stimulation (TMS)
Discussion
Nardone et al. (2014) completed a double blinded, sham controlled crossover RCT to evaluate the disynaptic reciprocal primary inhibition (i.e., mediated via pathway of muscle spindle 1a afferent to motoneurones of the antagonist muscle) of the soleus motoneurons in SCI study subjects. Study subjects were randomly allocated to receive either real rTMS (n=4) or a sham rTMS (n=5). Treatment was conducted daily over five days with real rTMS patients receiving two second duration bursts at 20 Hz with an interstimulus interval of 28 seconds for a total of 1600 pulses over 20 minuntes at an intensity of 90% of the resting motor threshold. After a four-week washout period, study subjects were crossed over, although only four of the five sham rTMS patients received real rTMS. Assessments were conducted at baseline and at initial, final, and one-week follow-up visits using the MAS, Spinal Cord Injury Assessment Tool for Spasticity (SCATS), monosynaptic test reflex responses (H-reflex), maximal H-reflex response (H-max), and maximal soleus motor action. Study results showed that spasticity was significantly reduced after real rTMS intervention, as measured by both MAS (p=0.0013) and SCATS (p=0.0008). MAS and SCATS values significantly decreased after the first treatment session (MAS: p<0.0001; SCAT: p<0.0001). MAS and SCAT scores at one-week follow-up were still significantly lower than baseline scores (MAS: p=0.0006; SCAT: p=0.0002). H-max/M-max ratio did not change significantly over the four assessments (p=0.17) among study subjects (controls not assessed for H-max/M-max). Reciprocal inhibition, according to H-reflex responses, was significantly modified in study subjects during real rTMS intervention (p=0.00004) compared to healthy controls. The conditioned H-reflex response significantly decreased after the first treatment session and from first to last treatment sessions (both p<0.0001). Conditioned H-reflex responses at one-week follow-up were still significantly lower than baselines scores (p<0.0001). The results of this study support and extend previous findings demonstrating the effects of rTMS on spasticity in SCI individuals.
Similarly, Benito et al. (2012) completed a double-blind sham controlled RCT (rTMS n=7, sham n=10) to study the effects of rTMS on spasticity in SCI. Three patients who received sham rTMS were crossed-over to receive real rTMS three weeks after completing the sham protocol. Real rTMS patients received two second bursts at 20 Hz (40 pulses/burst) with intervals of 28 seconds, for a total of 1800 pulses over 20 minuntes. The intensity of stimulation was set at 90% of the resting motor threshold. The study demonstrated that real rTMS resulted in significantly less spasticity according to MAS scores at the end of the last treatment session compared to baseline (p=0.027), but sham rTMS did not (p=0.066).
Kumru et al. (2010) examined the efficacy of rTMS on 15 individuals with incomplete SCI. rTMS was applied in two-second bursts at 20 Hz (40 pulses/burst) to the primary motor cortex over five days. Spasticity was significantly reduced at the end of the first and the last treatment sessions from both lower extremities when compared with the baseline condition as measured by the MAS (p<0.006). Additionally, unsolicited disclosures of improved sleep quality were reported by patients. These results remained one week post-treatment.
Nardone et al. (2015) completed a systematic review of published articles between 1966 and 2014 (n=49) using the MEDLINE, EMBASE Databases with no language and research design restrictions. Only articles reporting data on studies using Transcranial Magnetic Stimulation (TMS) and repetitive TMS (rTMS) on individuals with SCI were included. Nardone et al. (2015) sought to examine the effectiveness of TMS/rTMS as a clinical tool after SCI and examine the use of TMS/rTMS techniques to observe and map neural mechanisms and cortical excitability post-SCI. Two studies revealed significant improvements in spasticity; in particular, focusing treatment on leg motor areas of the brain was found to improve walking speed and spasticity of lower limbs. Additionally, pain relief was also reported post rTMS treatment.
Sub-threshold TMS can also be used to study the mechanisms of reorganisation processes by inhibiting outgoing electromyography readings. As well, TMS can enable mapping of motor cortical output by accurately assessing the number of cortical sites eliciting evoked potentials for a target muscle. Nardone et al. (2015) recommended that further studies are required to assess the safety and efficacy of TMS/rTMS as one study suggested that high levels of stimulation are required to obtain motor cortical excitability which can then induce discomfort and pain in the patient.
Conclusions
There is level 1a evidence (from two RCTs and one case control: Nardone et al. 2014; Benito et al. 2012; Kumru et al. 2010) that rTMS decreases spasticity and improves walking speed.

