Wearable Powered Exoskeletons for Standing Balance
Newer generations of exoskeletons, known as overground exoskeletons, are designed with portable systems that allow the user to ambulate freely indoors and outdoors (Yip et al. 2022). Wearable exoskeletons or robotic orthoses are other terms that are used interchangeably for these robotic devices, which are wearable and operate in the close proximity of the joints of patients (Jamwal et al. 2020). Activation of these systems can be triggered by patients’ voluntary movements or by a computer algorithm, depending on the patients’ capabilities and the exoskeleton characteristics (Rodriguez-Tapia et al. 2022).
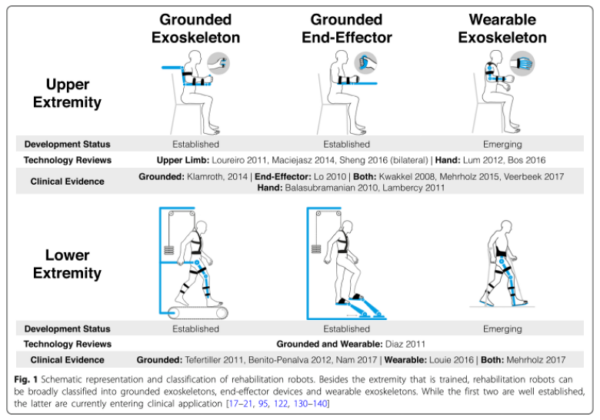
Figure 2. Schematic representation and classification of rehabilitation robots. From Gassert & Dietz 2018. Creative Commons license: https://creativecommons.org/licenses/by/4.0/. No changes have been made.
Wearable powered exoskeletons differ from other RAGT systems because they offer new possibilities and key advantages in gait rehabilitation: first, wearable powered exoskeleton allows self-balancing, overground, gait training, with or without upper limb assistance; second, assistance during gait can be triggered voluntarily by the participant through muscle contraction and body movements; third, gait training, through TSR, can be performed in more ecological environments, promoting a more human-like gait pattern (including activation of trunk muscles during over ground or treadmill training); fourth, they are not limited to a laboratory or clinic setting, and users can wear them in community and home settings, providing opportunities to practice walking outside of a clinical environment; and finally, wearable powered exoskeletons enable walking with a lower energetic cost compared to other systems (Heinemann et al. 2020; Rodriguez-Tapia et al. 2022).
The number of studies on wearable exoskeletons during the past 10 years has seen a rapid increase, following the general tendency now towards rehabilitation robots (Esquenazi & Talaty 2019). The systematic review of Rodríguez-Fernández et al. (2021) identified 25 wearable lower-limb powered exoskeletons for overground training, without BWS, that have been tested for use with people who have gait disorders due to neuromuscular impairments (e.g., SCI, stroke, and other pathologies). From this number, only six have FDA approval and/or CE mark and are commercially available (i.e., Ekso, HAL, Indego, REX, ReWalk, and SMA) (Rodríguez-Fernández et al. 2021).
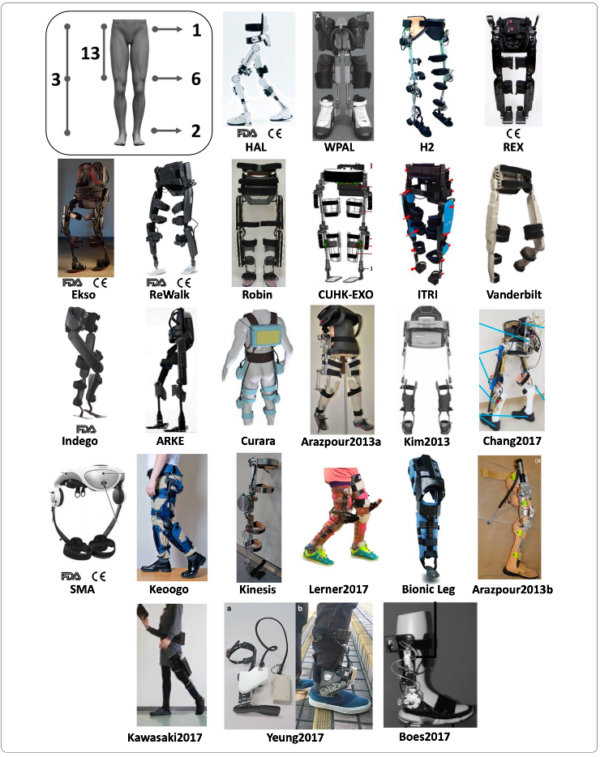
Figure 3. Exoskeletons included in the literature review of Rodríguez-Fernández et al. 2021. From Rodríguez-Fernández et al. 2021. Creative Commons license: https://creativecommons.org/licenses/by/4.0/. No changes have been made.
Currently, exoskeletons can be subdivided into assistive devices to be used in the community, such as the Indego Personal and Rewalk exoskeletons, or devices designed for rehabilitation with a therapeutic intent, such as the EksoNR and Indego Therapy exoskeletons (Yip et al. 2022). Nowadays, for patients with tetraplegia, FDA has approved three devices: Ekso® (allowed only for C7–T3 AIS D patients), Indego® (C7 or below) and Hal® (C4–L5 AIS C or D) (Rodriguez-Tapia et al. 2022). These three exoskeletons can be used after SCI if upper limb strength is enough to allow the use of assistive devices, such as crutches or walkers (Rodriguez-Tapia et al. 2022). Other self-balancing wearable powered exoskeletons, like Atalante® or Rex®, allow ambulation without upper limb help or the use of an assistive device (Postol et al. 2021; Rodriguez-Tapia et al. 2022). Studies which assessed the effects on balance outcomes in trials after the use of these exoskeletons; as well as others such as the ABLE Exoskeleton, the AIDER (AssIstive DEvice for paRalyzed patient) powered robotic exoskeleton, the reWalk wearable lower limb powered exoskeleton, the Achilles exoskeleton, the ExoAtlet Medy®, the Erigo, and the H-MEX (Hyundai Medical Exoskeleton) have been included in the present section.
It could be necessary to know which patients would benefit the most from receiving exoskeleton training, as learning to use an exoskeleton is time-consuming, and the number of training sessions required to walk independently differs greatly between users (van Dijsseldonk et al. 2021). 20 participants with motor complete SCI received 24 training sessions in eight weeks with a ReWalk exoskeleton, and lesion level appeared to be an important predictor during the first four weeks of training, but did not influence participants’ final skill level, while body mass index, age, and active lifestyle were predictors of exoskeleton skill performance toward the end of the training period (van Dijsseldonk et al. 2021).
Discussion
There is understandable excitement around the proliferation of exoskeleton technologies for regaining the ability to stand and ambulate (Fritz et al. 2019). Despite the promising results and enthusiasm regarding robotic exoskeletons’ potential, there are still several limitations to their use as a rehabilitation therapy tool and as a personal mobility device, such as device safety, set-up requirements, slow speeds for community ambulation, level and completeness of injury, body composition and weight, range of motion required for use, and high cost (Heinemann et al. 2020; Gorgey 2018). Interestingly, van Dijsseldonk et al. (2021) studied the validity of some parameters as predictors of performances related to the use of the ReWalk device, in people with chronic SCI. Factors such as an active lifestyle, young age at the time of the injury, low lesion level and low body mass index were found to be factors significantly correlated to the achievement of required motor tasks during training (i.e., maintenance of upright position and walking) (van Dijsseldonk et al. 2021). As previously shown in BWSTT intervention, the time since injury seems to be a predictor of the recovery of ambulation in exoskeleton-assisted training. One pre-post study assessed a gait training protocol using the exoskeleton Ekso in 52 participants with SCI who were subgrouped according to the time since injury (Baunsgaard et al. 2018a; Baunsgaard et al. 2018b). It was shown that after 8 weeks of training, the recently injured participants (n=25) significantly improved 10MWT, LEMS, TUG and BBS from baseline; while the chronically injured (n=27) showed a significant improvement only in TUG and BBS scores; with these changes being retained at four weeks of follow-up (Baunsgaard et al. 2018a; Baunsgaard et al. 2018b). However, according to the meta-regression analysis of Zhang et al. (2022), for comparing baseline demographic and clinical characteristics, it was shown that age, time after injury, and the AIS score had no impact on the outcomes of patients undergoing wearable EAW and Lokomat training.
Recent systematic reviews have been conducted to assess the safety, feasibility, and effects on gait and/or standing balance performance (and other health outcomes) of the use of different overground powered lower limb exoskeletons in patients with SCI (Duddy et al. 2021; Federici et al. 2015; Lajeunesse et al. 2015; Louie et al. 2015; Rodriguez-Tapia et al. 2022; Shackleton et al. 2019; Tamburella et al. 2022; Zhang et al. 2022). In a systematic review, Rodriguez-Tapia et al. (2022) found, from 570 participants with SCI who had been included, a total of 174 AEs, with a significantly higher occurrence in a population with paraplegia (n=157, 90%) compared to the population with tetraplegia (n=17, 10%). The systematic review of Tamburella et al. (2022) also showed that from the 41 studies included, 13 reported different AEs during training with exoskeletons. It was noted that the most frequent AEs were skin lesions, while the less frequent ones were the presence of extreme fatigue, falls, bone fractures or muscle strains (Tamburella et al. 2022). However, these and other results from Table 13, show that gait training using wearable powered exoskeletons may be a safe intervention after paraplegia (Miller et al. 2016) and tetraplegia (Rodriguez-Tapia et al. 2022).
Regarding standing balance outcomes, the systematic review and meta-analysis of Shackleton et al. (2019) included seven studies which studied over-ground robotic locomotor training and showed for TUG, a positive pooled effect of 0.74 (95% CI 0.36, 1.11) with no heterogeneity (I2 = 0%, p=0.0001). To date, the only network meta-analysis of RCTs and non-RCTs to assess the clinical effects (i.e. 10MWT, WISCI II, and TUG) of two different types of RAGT (Lokomat and wearable EAW) in patients with SCI was conducted by Zhang et al. (2022). It was shown that TUG scores were significantly improved from baseline by using wearable EAW [1.19 (95% CI=0.74, 1.64); I2=44%]. However, these (and other) benefits need to be confirmed through RCTs with larger sample sizes and higher quality because the small number of studies with a control group did not allow to establish if the benefits deriving from the use of exoskeletons are greater or lesser than conventional physical therapy (Duddy et al. 2021; Shackleton et al. 2019; Tamburella et al. 2022).
Regarding training dosage, Shackleton et al. (2019) showed that the most common intervention length was eight weeks and typically, training was conducted three times per week for 60 min per session; but there is still some degree of variability in training dosage according to other systematic reviews (Fang et al. 2020; Rodriguez-Tapia et al. 2022; Shackleton et al. 2019; Tamburella et al. 2022).
In line with previous systematic reviews published until the date assessing gait interventions with the use of exoskeletons (Rodriguez-Tapia et al. 2022; Tamburella et al. 2022; Shackleton et al. 2019), the two most studied exoskeletons models in people with SCI for standing balance outcome measures and falls assessed in this section are the Ekso® (Baunsgaard et al. 2018a; Baunsgaard et al. 2018b; Chang et al. 2018; Edwards et al. 2022; Hong et al. 2020; Sale et al. 2018; Sale et al. 2016; Kolakowsky-Hayner et al. 2013) and the ReWalk (Benson et al. 2016; Hong et al. 2020; Platz et al. 2016). Despite the promising results overall described, only a few high-quality studies have been conducted, comparing locomotor training interventions using exoskeletons with other locomotor interventions.
One high-quality study compared the use of a wearable exoskeleton with a traditional orthosis (Rodríguez-Fernández et al. 2022). The cross-over RCT of Rodríguez-Fernández et al. (2022) included 10 patients with chronic motor-complete and thoracic SCI who performed two overground training programs (with sit-to-stand and stand-to-sit transitions, and standing and walking exercises using one of the two devices [KAFO vs. ABLE exoskeleton]) of 10 sessions of 90 min duration. At the end of the study, it was shown that walking with the robotic device improved gait kinematics and spatiotemporal parameters compared to walking with knee ankle foot orthoses (KAFOs) (Rodríguez-Fernández et al. 2022). However, the performance during the clinical evaluations (6MWT, 10MWT, and TUG) and the energy consumption were similar (p > 0.05) (Rodríguez-Fernández et al. 2022). These results are of interest, as traditional orthoses represent a more accessible option than exoskeletons in people with SCI. Future studies comparing training interventions using these devices would be necessary to elucidate whether both devices provide similar improvements in standing balance outcomes or, on the contrary, one of them provides larger improvements in this function.
The RCT of Edwards et al. (2022) included 25 participants with chronic motor incomplete SCI who were randomly assigned to one of three interventions (i.e., Ekso robotic standing/up and walking and, if possible, overground training without BWS; BWSTT, and again, if possible, overground training without BWS; and continuing with daily activities as normal). After 12 weeks of training, gait speed (10MWT), walking endurance (6MWT), and standing balance (TUG test) improved in each of the three groups, with the highest improvements shown in the Ekso group, but without reaching statistical significance (Edwards et al. 2022). The authors stated that with a larger sample size, the promising results of the intervention with the Ekso exoskeleton might have appeared (Edwards et al. 2022).
The prospective controlled trial of Tamburella et al. (2020b) aimed to provide more data after promising results in gait speed, walking endurance and standing balance in four participants with incomplete motor SCI shown in the pre-post study of Tamburella et al. (2020a). Tamburella et al. (2020b) assessed the effects on gait and balance of a training program based on standing balance and gait training using the Achilles ankle exoskeleton (or not) for 10 sessions in eight patients with incomplete motor SCI. At the end of the training, there were significant improvements in spatio-temporal parameters (gait speed, gait cycle time, and step length) only for the experimental group; similar but not significant improvements in standing balance and manual muscle testing were shown in both groups (Tamburella et al. 2020b). These two studies are the only ones included in the present systematic review which assessed the effects of an ankle exoskeleton (developed to assist plantar/dorsiflexion during walking) for standing balance and walking performance; being of particular interest because the rest of the exoskeletons traditionally provide assistance reaching the lumbar/pelvis/hip joints. More research on interventions for improving standing balance, focusing on the ankle joint and muscle groups, could be important to carry out. For example, it has been shown that ankle muscle activity co‐contractions may be a compensatory strategy for individuals with incomplete SCI to accommodate for decreased motor function, but co‐contractions may result in increased ankle mechanical joint stiffness and consequently postural sway (Fok et al. 2021); or that individuals with incomplete SCI show larger postural sway compared with participants without SCI during quiet standing, primarily due to larger ankle joint acceleration (Lee et al. 2021).
Conclusions
There is level 1 evidence (from 1 RCT: Rodríguez-Fernández et al. 2022) that an overground training program with the ABLE exoskeleton provides a better improvement in gait kinematics and spatiotemporal parameters, but similar improvement in performance (6MWT, 10MWT, and TUG) compared to a training program with KAFOs in patients with chronic motor-complete and thoracic SCI.
There is level 2 evidence (from 1 RCT: Edwards et al. 2022) that walking training with an Ekso exoskeleton provides similar benefits in gait speed (10MWT) and endurance (6MWT), and standing balance (TUG test) than a BWSTT in patients with chronic motor incomplete SCI.
There is level 2 evidence (from 1 RCT: Chang et al. 2018) that three weeks of conventional physical therapy designed to facilitate gait improvement, but not exoskeleton-assisted gait training, provides significant improvements in standing balance (TUG) in people with incomplete and chronic SCI.
There is level 2 evidence (from 1 prospective controlled trial: Tamburella et al. 2020b) that the use of an NeuroMuscular Controller-controlled Achilles exoskeleton during 10 sessions of gait and balance training provides more improvements in walking distance (6MWT), but does not provide better improvement in lower limb strength (LEMS) nor standing balance (BBS), than the same training program performed without the use of the ankle exoskeleton, in patients with chronic and motor incomplete SCI.
There is level 4 evidence (from several pre-post studies) that wearable exoskeletons can enable safe walking and improvements in walking function and standing balance (TUG, BBS, among other outcome measures) in patients with SCI and different levels of injury (mostly paraplegia), AIS level, or time since injury (mostly chronic).
