Body-Weight Supported Treadmill Training (BWSTT) for Standing Balance
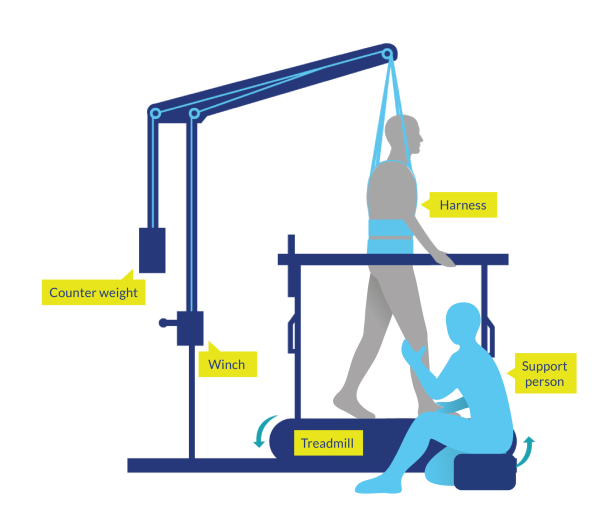
Figure 1. Body-Weight Supported Treadmill Training (BWSTT)
Discussion
Acute SCI (<1 year)
Eight studies have examined the effect of Lokomat-assisted or therapist-assisted BWSTT in people who had incurred an incomplete SCI <12 months prior (acute/subacute phase) (aggregate N=534) (Dobkin et al. 2006; Harkema et al. 2012; Midik et al. 2020; Schwartz et al. 2011; Shahin et al. 2017; Shin et al. 2014; Tang et al. 2014; Wirz et al. 2017) and one (Schwartz et al. 2011) in people who had incurred a complete SCI <12 months prior (acute/subacute phase) (N=6). Treatment time ranged from 90-300 min per week, and total treatment duration lasted between 4 and 12 weeks.
A good quality single-blind RCT (Dobkin et al. 2006) (n=117) showed no differences in effects between matched amounts of BWSTT with therapist assistance and overground mobility practice in incomplete SCI during inpatient rehabilitation for the locomotor score of the FIM, overground walking speed, or balance scores.
Although there is some evidence (from a case-control study) that the use of Lokomat-assisted BWSTTT in combination with conventional therapy provides better functional independence scores (SCIM) than conventional therapy alone in patients with acute SCI (Schwartz et al. 2011); there are other RCTs, case-control studies, and prospective controlled trials which showed similar improvements in standing balance (BBS), ambulation ability (Functional Ambulation Category), or functional independence (SCIM-III) for BWSTT plus conventional therapy and conventional therapy only (Midik et al. 2020; Schwartz et al. 2011; Shahin et al. 2017; Shin et al. 2014).
The effect of time of BWSTT sessions on mobility is a variable which has been studied in participants with SCI. The randomized, controlled, multicenter trial of Wirz et al. (2017) assessed the differences between a BWSTT intervention program using Lokomat with a 50-minute walking session versus a 25-minute walking session. After 8 weeks of intervention, both groups significantly improved the SCIM mobility subscore, but the intervention group improved more (without statistical analysis done between groups) than the control group (Wirz et al. 2017), suggesting that an intensive locomotor program could be feasible and beneficial in patients with acute SCI.
Chronic SCI (>1 year)
We found 11 RCTs (Alexeeva et al. 2011; Duffell et al. 2015; Labruyere & van Hedel 2014; Lam et al. 2014; Niu et al. 2014; Piira et al. 2019a; Piira et al. 2019b; Wu et al. 2012; Wu et al. 2016; Wu et al. 2018; Yang et al. 2014), six prospective controlled trials (Behrman et al. 2012; Buehner et al. 2012; Lorenz et al. 2012; Lin et al. 2020; Lin et al. 2022; Musselman et al. 2009), and 13 pre-post studies that altogether studied 1295 persons with complete and incomplete SCI, with chronicity ranging from 1 to 18 years post-injury. Treatment intensity ranged from 45 to 450 min per week, and treatment duration lasted between 3 and 18 weeks.
In a recent systematic review and meta-analysis, Benn et al. (2025) included a total of 26 studies with 500 participants describing and comparing the efficacy and dosage of interventions targeting upright balance control, balance confidence, and falls for adults with motor-incomplete SCI. There was a significant pooled effect for improvement in upright balance control (measured by BBS: Hedge’s g=.51; 95% CI, .36-.66; I2=.60; measured by FTSTS: Hedge’s g=.73; 95% CI, 1.18 to .27; I2=.99) and balance confidence (measured by the ABC Scale: Hedge’s g=.40; 95% CI, .13-.67; I2=.56) (Benn et al. 2025). The authors stated however, that the quality of the evidence of the included studies was low or very low; that there was a lack in those balance interventions targeting the cognitive strategies, static stability, and reactive postural control; and that there was no relationship between intervention dosage and balance-related outcomes (Benn et al. 2025). Similar results were found in the systematic review and meta-analysis completed by Walia et al. (2023), which included ten RCTs (n=222) and 15 pre-post trials (n=967) assessing people with incomplete SCI. Pooled SMD for controlled and uncontrolled trials of body-weight supported training interventions of -0.26 (95% CI, -0.70 to 0.18; p=0.25) and 0.46 (95% CI, 0.33 to 0.59; p<.001), respectively (Walia et al. 2023). The authors stated the need for further well-designed and appropriately powered RCTs to evaluate specific features of training interventions to improve standing balance function in incomplete SCI (Walia et al. 2023).
Overall, most of the studies included showed some improvements in standing balance, in particular for groups with better baseline walking ability, whether locomotor training was provided with a treadmill or performed over ground, body-weight supported, or involved other variations on walk-based therapies (e.g., overground gait training with obstacles, robot-applied resistance). Two good-quality RCTs (Piira et al. 2019a; Piira et al. 2019b) used BWSLT (overground and on a treadmill) with manual assistance, and robot-assisted locomotor training (with the use of Lokomat®), respectively, in patients with motor incomplete SCI. Improvements in walking outcomes, standing balance, and strength were small and non-significant in the intervention groups, without differences between groups. An RCT by Niu et al. (2014) showed that Lokomat training in participants with low walking capacity at baseline did not show significant improvements, in contrast with participants with a high walking capacity who presented a consistent linear trend in time for both speed and functional balance (TUG) over the 4-week training period.
Longer periods of training on body-weight supported training also produced mixed results in balance outcomes for people with SCI. In an RCT, Alexeeva et al. (2011) included 35 participants with incomplete SCI who were randomly allocated to receive different ambulation therapy interventions. After 13 weeks of intervention, the physical therapy skill training and body-weight supported ambulation on a fixed track groups resulted in greater balance improvements than body-weight supported ambulation on a treadmill (Alexeeva et al. 2011). Labruyere and van Hedel (2014) included 9 participants with incomplete SCI who received RAGT with Lokomat or strength training. After 16 sessions, there were no statistical differences between the interventions with respect to the changes in standing balance scores (measured by BBS) (Labruyere & van Hedel 2014). Other lower evidence (pre-post) studies showed contradictory results, as some provided significant improvements in balance outcomes (normalized jerk values [instrumented sway test], TUG, BBS) (Covarrubias-Escudero et al. 2019; Fritz et al. 2011; Varoqui et al. 2014) and others did not (Knikou et al. 2013).
Alternative gait retraining therapies or modified approaches to BWSTT for chronic SCI are being introduced (Fleerkotte et al. 2014; Lam et al. 2014; Musselman et al. 2009; Wu et al. 2012; Wu et al. 2016; Wu et al. 2018; Yang et al. 2014). Musselman et al. (2009) and Yang et al. (2014) compared BWSTT with overground ‘precision’ skilled walking training. The skilled walking training consisted of task-specific practice (without WBS) of various gait tasks, such as stair climbing, obstacle crossing, and walking along sloped surfaces. Both training groups were comparable in improving standing balance (measured by the BBS and the ABC scale). Wu et al. (2012; 2016) demonstrated a new cable-driven robotic device to apply resistance against leg movements during BWSTT. Participants were randomized (in a cross-over design) to receive robotic resistance or BWSTT. Although there were no significant differences in outcomes between the two modalities (Wu et al. 2012; Wu et al. 2016), there was some indication that robotic resistance enabled greater gains in over ground walking speed and standing balance (BBS) in people who tended to have better initial ambulatory capacity (Wu et al. 2012). Wu et al. (2018) studied the same training program (assistive robotic BWSTT) and compared it with a BWSTT alone (no assistance), in the same way as in the previous studies, no changes were shown in standing balance as measured by the BBS or the ABC scale after 6 weeks of both training programs in people with incomplete SCI. The RCT of Duffell et al. (2015) compared the effects of a BWSTT intervention with Lokomat and a pharmacological drug for treating spasticity (Tizanidine). After four weeks, there were no significant effects between both groups in standing balance (TUG) (Duffell et al. 2015).
There were three studies which tried to assess the effects on balance (weight shifting) and gait (stepping) of the application of pelvis assistance (Lin et al. 2019), perturbation force (Lin et al. 2020), or perturbation force plus transcutaneous spinal direct current stimulation (Lin et al. 2022) during single sessions of treadmill walking with a customized cable-driven robotic system in people with chronic and incomplete SCI. Overall, the authors showed that applying pelvis assistance during treadmill walking may facilitate weight shifting and improve step length (which may partially transfer to overground walking) (Lin et al. 2019); that dynamic balance control capacity (calculated by margin of stability, weight shifting, and other spatiotemporal gait parameters) was improved after 10 min of treadmill walking paired with the application of a varied pelvis perturbation force (Lin et al. 2020); and that anodal transcutaneous spinal direct current stimulation may modulate motor adaptation to pelvis perturbation and facilitate learning of dynamic balance control (measured by the minimal margin of stability) (Lin et al. 2022). Despite these promising effects on dynamic balance and gait kinematics outcomes, more studies are needed using functional balance and gait outcomes (e.g., 6MWT, 10MWT, TUG, WISCI and/or BBS), and with long-term training interventions, to confirm these promising results in people with chronic and incomplete SCI.
There is variability in studies we found in the percentage of bodyweight that supported each participant during BWSTT; ranging from ≤ 40% (Alexeeva et al. 2011; Labruyere & van Hedel 2014; Piira et al. 2019a; Piira et al. 2019b), 50% (Okawara et al. 2020), to 60% (Knikou 2013). In other cases, the BWS was set individually to provide as much support as necessary to prohibit knee buckling or toe drag during stepping, or adjusted to the minimum tolerated by the participant while ensuring appropriate stance phase kinematics (Covarrubias-Escudero et al. 2019; Lam et al. 2014; Musselman et al. 2009; Varoqui et al. 2014; Wu et al. 2012; Yang et al. 2011). All studies progressively decreased the amount of bodyweight supported depending on the participant’s tolerance during the training period. As the authors are aware, there is no study published comparing the effects of different percentages of BWS on standing balance in patients with SCI. However, the RCT of El Semary and Daker (2019) compared 30% vs. 40% of BWS in patients with motor-incomplete SCI and paraplegia. After 6 weeks of BWSTT performed twice a week, walking speed, step length, stride length and cadence width (but not step width) were improved in both groups, but between-group comparisons revealed that there were highly significant changes in these parameters for the group who trained with a 40% of BWS (El Semary & Daker 2019).
Conclusions
Acute SCI (<1 year)
There is level 1 evidence (from 1 RCT: Dobkin et al. 2006) and level 2 evidence (from 2 RCTs: Midik et al. 2020; Shin et al. 2014; and from 1 prospective controlled trial: Shahin et al. 2017) that BWSTT has equivalent effects to conventional rehabilitation consisting of an equivalent amount of overground mobility practice for standing balance (BBS) and functional independence (SCIM) outcomes in patients with acute/sub-acute SCI.
There is level 1 evidence (from 1 RCT: Wirz et al. 2017) that intensive sessions (walking time per session > 50 min) of Lokomat-assisted BWSTT for 8 weeks were tolerable and could provide more improvement in SCIM mobility subscore than non-intensive Lokomat-assisted BWSTT sessions (walking time per session < 25 min) in patients with acute SCI.
There is level 3 evidence (from 1 case control study: Schwartz et al. 2011) that 12 weeks of BWSTTT with Lokomat in combination with conventional therapy provides significant and better functional independence scores (SCIM) than conventional therapy alone in patients with acute, complete and incomplete SCI.
Chronic SCI (>1 year)
There is level 1 evidence (from 1 RCT: Alexeeva et al. 2011) that physical therapy skill training and body-weight supported ambulation on a fixed track provides greater balance (Tinetti scale) improvements than body-weight supported ambulation on a treadmill in patients with chronic and incomplete SCI.
There is level 1 evidence (from 1 RCT: Labruyere & van Hedel 2014) that four weeks of a RAGT with Lokomat provides similar improvements in standing balance (BBS) as a strength training program in patients with incomplete and chronic SCI.
There is level 1 evidence (from 1 RCT: Piira et al. 2019a) that BWSLT with manual assistance does not provide more improvements than usual care in standing balance (BBS) in patients with chronic and motor incomplete SCI.
There is level 1 evidence (from 1 RCT: Piira et al. 2019b) that robot-assisted locomotor training (with LokomatÒ), compared to usual care, does not provide better improvements in standing balance (BBS) in patients with chronic SCI.
There is level 1 (from 1 RCT: Yang et al. 2014) and level 2 evidence (from 1 prospective controlled trial: Musselman et al. 2009) that BWSTT or overground ‘precision’ skilled walking training provides similar improvements in standing balance (measured by the BBS and the ABC scale) in participants with chronic SCI.
There is level 1 evidence (from 1 RCT: Wu et al. 2018) that a 6-week BWSTT with assistance (using a cable-driven robotic device to provide bilateral pelvis assistance load) does not provide improvements in standing balance (BBS and ABC scale) in the same way that a BWSTT only (no assistance) in people with incomplete and chronic SCI.
There is level 2 evidence (from 2 cross-over RCTs: Wu et al. 2012; Wu et al. 2016) that a BWSTT with assistance or resistance (using a cable-driven robotic device to apply resistance against leg movements during BWSTT) provides similar effects after 6-8 weeks in standing balance (BBS and ABC scale) in people with incomplete and chronic SCI.
There is level 2 evidence (from 1 RCT: Duffell et al. 2015) that BWSTT (with Lokomat) or Tizanidine (a pharmacological drug for treating spasticity) does not provide significant improvement in standing balance (TUG) after four weeks of intervention in people with chronic SCI.
There is level 4 evidence (from 14 pre-test/post-test studies: Behrman et al. 2012; Buehner et al. 2012; Covarrubias-Escudero et al. 2019; Fleerkotte et al. 2014; Fritz et al. 2011; Harkema et al. 2012; Lorenz et al. 2012; Varoqui et al. 2014) that BWSTT (with different approaches) is effective for improving standing balance performance in people with chronic and incomplete SCI.
There is level 4 evidence (from 4 pre-post studies: Aach et al. 2014; Jansen et al. 2017; Okawara et al. 2020; Sczesny-Kaiser et al. 2015) that a BWSTT program using the HAL exoskeleton provides improvements in balance (TUG) in patients with complete or incomplete and chronic SCI.
