Wearable Powered Exoskeletons (WPEs)
Wearable powered exoskeletons (WPEs) could be defined as computer-guided systems using motorized orthoses to facilitate autonomous overground movement in people with disabilities (Rodriguez-Tapia et al. 2022). WPE or robotic orthoses are other terms that are used interchangeably for these robotic devices, which are wearable and operate in the proximity of the joints of patients (Jamwal et al. 2022). Activation of these systems can be triggered by patients’ voluntary movements or by a computer algorithm, depending on the patients’ capabilities and the exoskeleton characteristics (Rodriguez-Tapia et al. 2022).
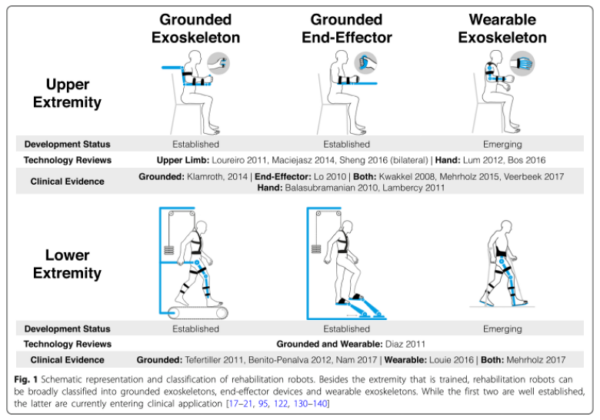
Figure 5. Schematic representation and classification of rehabilitation robots. From Gassert & Dietz 2018. Creative Commons license: https://creativecommons.org/licenses/by/4.0/. No changes have been made.
WPE differs from other RAGT systems because it offers new possibilities and key advantages in gait rehabilitation (Heinemann et al. 2020; Rodriguez-Tapia et al. 2022):
- WPE allows self-balancing, overground, and gait training, with or without upper limb assistance.
- Assistance during gait can be triggered voluntarily by the participant through muscle contraction and body movements.
- Gait training, through task-specific rehabilitation, can be performed in more ecological environments, promoting a more human-like gait pattern (including activation of trunk muscles during overground or treadmill training).
- Some WPE are not limited to a laboratory or clinic setting, and users can wear them in community and home settings, providing opportunities to practice walking outside of a clinical environment.
- WPE enable walking with a lower energetic cost compared to other systems.
In a systematic review, Rodríguez-Fernández et al. (2021) identified 25 wearable lower-limb powered exoskeletons for overground training that have been tested for use with people who have gait disorders due to neuromuscular impairments (e.g., SCI, stroke, and other pathologies). Only six of these have Food and Drug Administration (FDA) approval, are commercially available and regulated for use in the USA (i.e., Ekso, HAL, Indego, REX, ReWalk and SMA) (Rodríguez-Fernández et al. 2021; Onate et al. 2024).
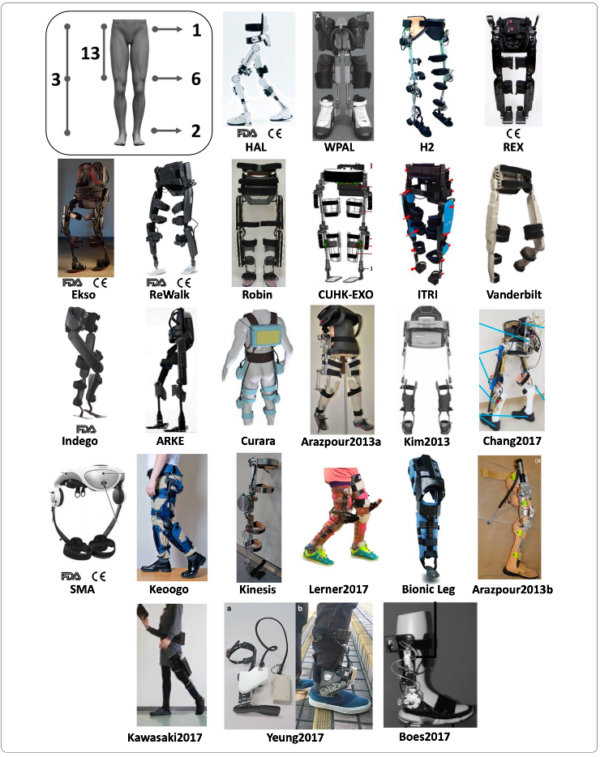
Figure 6. Exoskeletons included in the literature review of Rodríguez-Fernández et al. 2021. From Rodríguez-Fernández et al. 2021. Creative Commons license: https://creativecommons.org/licenses/by/4.0/. No changes have been made.
Discussion
The majority of the systematic reviews and meta-analyses testing WPE in people with SCI have shown improvements in walking speed, walking distance, and/or lower limb strength (Duddy et al. 2021; Moriarty et al. 2024; Shackleton et al. 2019; Tamburella et al. 2022; Zhang et al. 2022; Rodriguez-Tapia et al. 2022).
EXO vs. Physical Therapy (Usual Care)
Studies that we found comparing exoskeleton to conventional physical therapy or ‘usual care’ showed that both types of training improved walking outcomes in people with SCI. However, only a few higher-quality studies performed between-group analyses that show if one method is better than the other at helping people with SCI to regain walking ability.
Shackleton et al. (2024) compared the effects of robotic locomotor training to activity-based therapy (ABT) in people with SCI; they found that after 24 weeks, participants in both groups improved their functional walking (SCI-FAI) and lower extremity strength (LEMS), however, neither group significantly outperformed the other (Shackleton et al. 2024). Xiang et al. (2021) compared exoskeleton walking training versus strength training and aerobic exercise at similar intensities. After 4 weeks of training, patients in both groups improved similarly on walking distance (6MWT), but neither group showed improvements in LEMS (Xiang et al. 2021). However, Tsai et al. (2020) found that people who used a powered exoskeleton (EksoGT) had statistically significant improvements compared to patients who did not receive any walking training with exoskeleton during the acute inpatient rehabilitation.
EXO vs. OGT/BWSTT
Gil-Agudo et al. (2023) compared the effects of robotic locomotor training versus traditional gait training on walking to determine which method is superior at developing walking ability and lower limb strength in people with SCI. After 5 weeks, the exoskeleton group developed significantly more functional walking ability (e.g., higher WISCI-II scores) than the traditional gait training group. Both groups walked significantly further at the end of training (6MWT – Exo: +68 meters; OGT: +48 meters), but neither walked significantly further than each other. Both groups improved slightly LEMS and in walking speed (-.2m/s and -.1m/s) (Gil-Agudo et al. 2023).
Edwards et al. (2022) compared Ekso robot gait training to an active control group, who engaged in BWSTT, and a passive control group, who received no additional activities (i.e., usual PT). After 12 weeks, the proportion of participants with improvement in clinical ambulation category from home to community speed was greatest in the Ekso group (>1/2 Ekso, 1/3 Active Control, 0 Passive Control, p < 0.05). Self-selected gait speed following the 12-week intervention increased in the Ekso group by 51% (mean, SD; 0.18 ± 0.23 m/s) Active Control by 32% (0.07 ± 0.11 m/s) and Passive Control 14% (0.03 ± 0.03 m/s; all differences ns). The median distance covered in the 6MWT following the 12-week intervention was 538.0 feet for the Ekso Group, 346.6 feet for the Active Control, and 320.0 feet for the Passive Control (ns) (Edwards et al. 2022).
We found one network meta-analysis of RCTs and non-RCTs comparing BWSTT (i.e., Lokomat) to EAW on walking outcomes (Zhang et al. 2022). They found that of the studies aiming to develop walking speed (i.e., 10MWT) it was mostly likely for EAW to rank first (89%) and for Lokomat to rank second (47%), whereas in studies measuring functional walking (i.e., WISCI-II scores) it was mostly like for Lokomat to rank first (73%) and EAW to rank second (63%) (Zhang et al. 2022).
Which Type of Exoskeleton is Best?
There are few if any studies comparing one exoskeleton to another, likely due to the high cost of this type of walking technology. Currently, exoskeletons can be subdivided into assistive devices used in the community, such as the Indego Personal and Rewalk exoskeletons, or devices designed for rehabilitation with a therapeutic intent, such as the EksoNR and Indego Therapy exoskeletons (Yip et al. 2022). For patients with tetraplegia, the US FDA has approved three devices: Ekso® (allowed only for C7–T3 AIS D patients), Indego® (C7 or below) and Hal® (C4–L5 AIS C or D) (Rodriguez-Tapia et al. 2022). These three exoskeletons can be used after SCI if upper limb strength is enough to allow the use of assistive devices, such as crutches or walkers (Rodriguez-Tapia et al. 2022). Other self-balancing WPE, like Atalante® or Rex®, allow ambulation without upper limb help or the use of an assistive device (Postol et al. 2021; Rodriguez-Tapia et al. 2022).
Who for? How Much? How long?
van Dijsseldonk et al. (2021) studied the validity of some parameters as predictors of performance related to the use of the ReWalk device in people with chronic SCI. Factors such as an active lifestyle, younger age at the time of the injury, a lower lesion level, and a low body mass index were found to be factors significantly correlated to the achievement of required motor tasks during training (i.e., maintenance of upright position and walking) (van Dijsseldonk et al. 2021). However, according to the meta-regression analysis by Zhang et al. (2022), it was shown that age, time after injury, and the AIS score had no impact on the outcomes of patients undergoing wearable EAW and Lokomat training.
Regarding training dosage, Shackleton et al. (2019) showed that the most common intervention length was 8 weeks and typically, training was conducted three times per week for 60 min per session; however, there is still some degree of variability in training dosage according to other systematic reviews (Fang et al. 2020; Rodriguez-Tapia et al. 2022; Shackleton et al. 2019; Tamburella et al. 2022).
Limitations
There is understandable interest around the use of exoskeleton technologies for regaining the ability to stand and ambulate (Fritz et al. 2019). There are several limitations to exoskeleton use as a rehabilitation therapy tool and as a personal mobility device, such as device safety, set-up requirements, slow speeds for community ambulation, level and completeness of injury, body composition and weight, ROM required for use, high cost, and limited accessibility and availability for gait rehabilitation (Heinemann et al. 2020; Gorgey 2018; Herrera-Valenzuela et al. 2023).
Regarding safety, one systematic review by Duddy et al. (2021) reported that powered exoskeleton devices seem to be safe to use with patients with neurological impairments, with no serious AEs occurring. Conversely, two systematic reviews on exoskeleton trials in people with SCI documented an AE rate of 25-30%, with the most frequent AEs being skin lesions; less frequently occurring AEs were extreme fatigue, falls, bone fractures or muscle strains (Rodriguez-Tapia et al. 2022; Tamburella et al. 2022). Bass et al. (2022) developed an algorithm based on bone mineral density aimed at minimizing fracture risk for people with SCI engaging in exoskeleton walking training available here. Possible AEs should always be considered prior to exoskeleton walking training and appropriate caution should always be exercised.
There are multiple limitations to the research conducted to date on exoskeletons and people with SCI. Most studies established improvement in walking outcomes whether exoskeleton training or more conventional PT was employed; it would be most helpful to know whether the benefits deriving from the use of exoskeletons are greater or lesser than conventional physical therapy (Duddy et al. 2021; Shackleton et al. 2019; Tamburella et al. 2022). This could be established with additional RCTs, larger sample sizes, and clearer emphasis on between-group analyses.
Conclusions
There is level 1 evidence (from 1 RCT: Xiang et al. 2021) that walking training with an exoskeleton (AIDER exoskeleton) provides a similar benefit in gait endurance (6MWT) as strength and aerobic exercise training in patients with acute SCI.
There is level 1 evidence (from 1 RCT: Gil-Agudo et al. 2023) that robotic locomotor training (using the HANK exoskeleton) compared with traditional gait training for five weeks provides significant improvements in walking ability (WISCI II); but not in walking distance (6MWT), walking speed (10MWT), lower limb strength (LEMS), or functional independence (SCIM-III) in participants with acute and incomplete SCI.
There is level 1 evidence (from 1 RCT: Shackleton et al. 2024) that a 24-week program of walking training using an exoskeleton (EksoGT) compared to ABT provides similar benefits in LEMS and functional walking (SCI-FAI) in people with chronic incomplete SCI.
There is level 2 evidence (from 1 RCT: Edwards et al. 2022) that walking training with an exoskeleton (Ekso exoskeleton) compared to BWSTT and usual PT in people with chronic motor incomplete SCI provides significant benefits in functional ambulation (WISCI-II scores), but all groups had similar improvements in gait speed (10MWT) and walking distance (6MWT).
There is level 3 evidence (from 1 case control study: Tsai et al. 2020) that OWT with an exoskeleton (EksoGT) in comparison with usual care (not receiving any walking training with an exoskeleton), provides a significant improvement in LEMS in patients with acute or subacute (mean time since injury = 19.3 days) SCI during inpatient rehabilitation.
