Primary Care and Respiratory Management
Spinal cord injury (SCI) disrupts the innervation to muscles needed for breathing (sternocleidomastoid, diaphragm, pectoralis major and abdominals), especially in those with higher level injuries (i.e., cervical, C1-C5). This results in impaired breathing, fatigue, and limited ability to cough. Pneumonia, bronchitis, and sleep-disordered breathing are common in people with SCI, often resulting in re-hospitalization, so prevention and timely diagnosis are important. Common treatments are medication (e.g., bronchodilators), ventilation support, and physical therapy for breath training and/or cough assistance.
The level of SCI, and whether the injury is complete or incomplete, determines which respiratory muscles are affected, and thus, the complexity and the severity of ensuing respiratory problems.
If your patient is injured at:
- C1-C2 – All muscles required for breathing are denervated; life-long ventilation likely required.
- C3-C5 – Diaphragm is denervated, inhibiting about 70% of inhalation; patient may require ventilation though weaning has been successful at C3-C5. Patient probably will require physical therapy, respiratory training, and cough assistance.
- C6-C8 – Scalenes accessory and pectoralis major denervated; patient likely experiences more difficulty with expiration, muscle fatigue, and weak/ineffective cough so percussive therapy, physical therapy, or assisted cough may be necessary.
- T1–T12 – Intercostals and abdominal muscles affected; more trouble with expiration and weak/ineffective cough, so secretion management will be important.
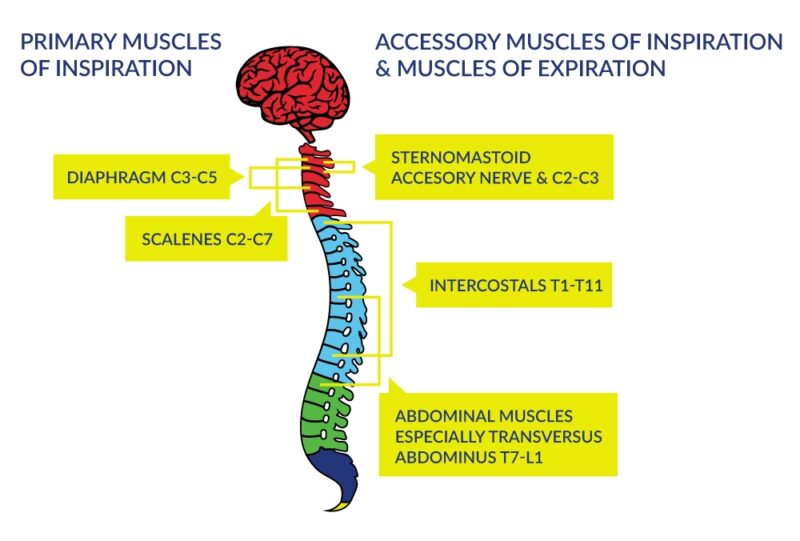
Figure 1. Innervation of the Respiratory Muscles
Recommendations for Respiratory Health Promotion
If your patient has any denervation of muscles involved in breathing, respiratory health promotion should be emphasized for your patient with SCI, including:
- Smoking cessation (including vaping or marijuana smoke) and staying away from secondhand smoke will be important. If your patient uses CBD for spasticity or pain control, it is preferable that it is not smoked.
- Staying up to date on vaccinations (e.g., flu, RSV, COVID-19) according to current guidelines.
- Staying hydrated to help ensure any mucus or secretions are thin. Generally, 2-2.5L of water per day is recommended.
- If there are pre-existing or concurrent conditions like COPD or asthma, then management will need to be especially assertive, taking into account your patient’s injury level (i.e., higher the injury = breathing and complications likely will be worse).
- Breathing while exercising is more difficult than quiet breathing; asking your patient about their exercise and physical activity, and how they maintain their breathing is a good idea to do regularly.
In addition:
- Listening to your patient’s lungs regularly is mandatory surveillance, particularly if your patient with SCI has a high level/complete injury. Listening for cracking/bubbling noises will be helpful to determine how well your patient is breathing and for catching illness early on, as well as for determining if additional support would be helpful (i.e., medication, respiratory therapies).
- Checking your patient’s ability to cough is similarly important. If their cough is weak/ineffective, you can ask how they clear secretions, which is key to preventing and treating respiratory infections.
- Asking your patient with SCI (and their partner/caregiver) about their sleep may be important also, as obstructive sleep apnea (OSA) is common in people with SCI. If they (or their partner/caregiver) report that they stop breathing at night, snore loudly, have restless sleep, wake up with a sore/dry throat and/or headache, of if they have daytime fatigue, they may be suffering from sleep apnea.
Respiratory Complications Are More Common in People with SCI
- Pneumonia and Respiratory Infections – It is common for colds/flus that have pulmonary congestion to be detected later and last longer in people with SCI (due to impaired sensation). Pneumonia (aspiration, community-acquired, and hospital/ventilator-associated) is one of the most common causes of re-hospitalization and mortality for people living with SCI; especially in complete tetraplegia. The risk for dysphagia and consequent aspiration pneumonia is also elevated in patients with cervical SCI.
- Sleep-Disordered Breathing – Sleep-disordered breathing (SDB) is much more common in patients with SCI (40-60%), especially if they have a higher level of injury, complete injury, are overweight, and are taking muscle relaxant medications. Obstructive sleep apnea (OSA) is far more common than central or mixed sleep apnea. OSA is also associated with a number of medical problems such as diabetes, heart attacks, heart failure, irregular heartbeat, high blood pressure, stroke, and depression.
Treatments
Medication
Pharmacologic secretion management may use mucoactive agents (e.g., expectorants, mucolytics) that are designed to either decrease mucus hypersecretion or increase the ability to expectorate the mucus. Bronchodilators may also be considered to improve lung volume. Any medication prescribed for your patient with SCI needs to consider other medications that they are on for possible interactions.
Mechanical/Physical Therapies
There are physical and mechanical therapies that can help people with SCI with their breathing and cough strength/secretion clearance if medication is not a preferred option.
- Physical Therapy (Breath Training) – Physiotherapy (PT) referral should be considered in all patients for respiratory muscle training (RMT) to improve breathing and coughing. Exercises will typically involve breath training, using a small pressurized device for developing inhaling and exhaling strength (called inspiratory or expiratory muscle training). Another common technique in physical therapy is called Breath Stacking, where a person uses a mouthpiece and a breath bag to ‘double inhale’, expanding the lung volume over time and use. Speech Language Pathology – Speech Language Pathologists (SLPs) often work jointly with PTs to determine the appropriate breathing exercises for people with SCI, but they have an additional focus of breath support for speech and for swallowing coordination (i.e., dysphagia).
- Manually Assisted Coughing – Manually assisted coughing (MAC or ‘quad cough’) requires assistance, but it can help a person with SCI cough and clear secretions without additional equipment. The patient maximally inhales, then coughs, while simultaneously a caregiver times an upward abdominal thrust below the diaphragm with the cough.
- Mechanical Insufflation–Exsufflation – Mechanical insufflation–exsufflation (MIE) is a commonly used and highly effective therapy for SCI to promote secretion clearance and augment breathing. The device simulates a cough by delivering a deep breath (pushing air into lungs) and then sucking the air back out (exhalation). Assistance by a caregiver is usually required to use the device and it can be used by ventilated and nonventilated persons.
- Percussive therapy – Chest wall percussion therapy uses vibration, manual chest therapy, or a percussive vest to loosen secretions for expectoration. Consider handheld continuous or oscillating positive expiratory pressure devices.
- Abdominal Binders – Abdominal binders are essentially wide bandage wraps with Velcro closures that go around the entire abdomen. They can assist with breath support, posture, balance, and blood pressure regulation. They need to be donned and doffed regularly to prevent compression injuries and skin breakdown.

(Clockwise from top left) Mechanical Insufflation/Exsufflation machine; Person using ‘The Breather’ ® Respiratory Muscle Trainer; two people performing Manual Assisted Coughing with person with SCI
Respiratory complications, like a cold/flu with excessive mucus that they have had for too long, will often present when immediate action is required.
- If your patient presents with cough and/or cold/flu like symptoms that have persisted, maintain a high level of suspicion for pneumonia and/or respiratory infection. Treat aggressively and immediately with appropriate medication, bed rest, and IV fluids/hospitalization if necessary.
- If your patient has a higher-level injury, or denervation to any respiratory muscles including the abdominals, you will want to ask about (and listen to) their breathing, coughing and inquire about sleep quality and fatigue at every appointment.
To a Respirologist/Respiratory Therapist ⇒ Lung Function Test
Lung function tests may be performed to evaluate lung capacity post-SCI. These measures help determine the degree to which respiration is impaired, the degree of ventilation the patient may require, and overall patient outcomes.
To a Physiotherapist and/or a Speech Language Pathologist ⇒ Respiratory Muscle Training
Physiotherapy (PT) referral should be considered in all patients for respiratory muscle training (RMT) for improvement of breathing and coughing.
Speech Language Pathologists (SLPs) often work jointly with PTs to determine the appropriate breathing exercises for people with SCI, but they have an additional focus of breath support for speech and for swallowing coordination (i.e., dysphagia).
To a Sleep Disorder Specialist ⇒ Sleep Disordered Breathing
If there are signs and symptoms of any sleep-disordered breathing, sleep studies will help determine the appropriate treatment options.
Polysomnography will help detect the presence of sleep apnea, but may be logistically difficult in the context of SCI. Most commonly, Continuous Positive Airway Pressure (CPAP) or Bi-level Positive Airway Pressure (BiPAP) machines are prescribed as the primary treatment for sleep apnea.
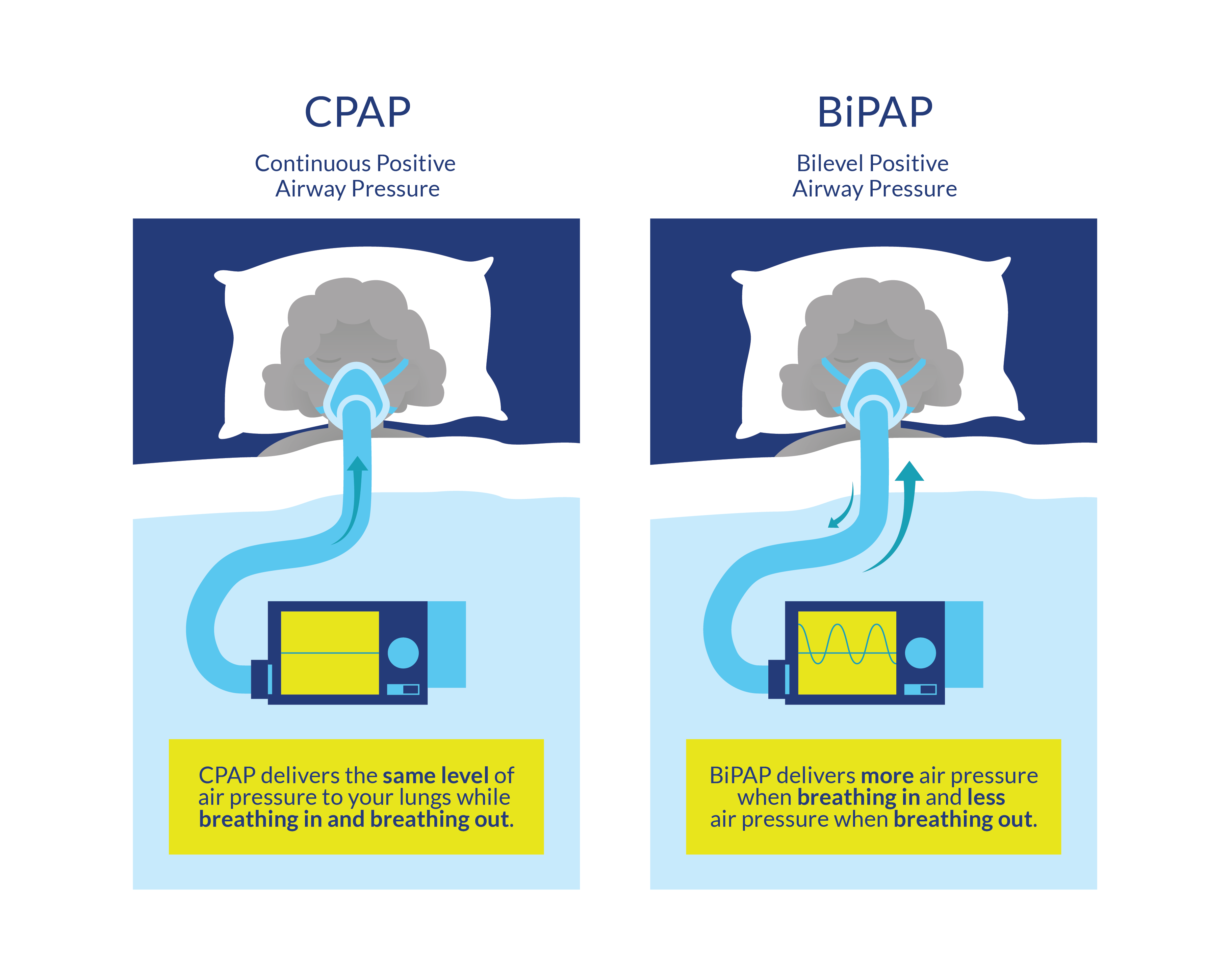
CPAP and BiPAP
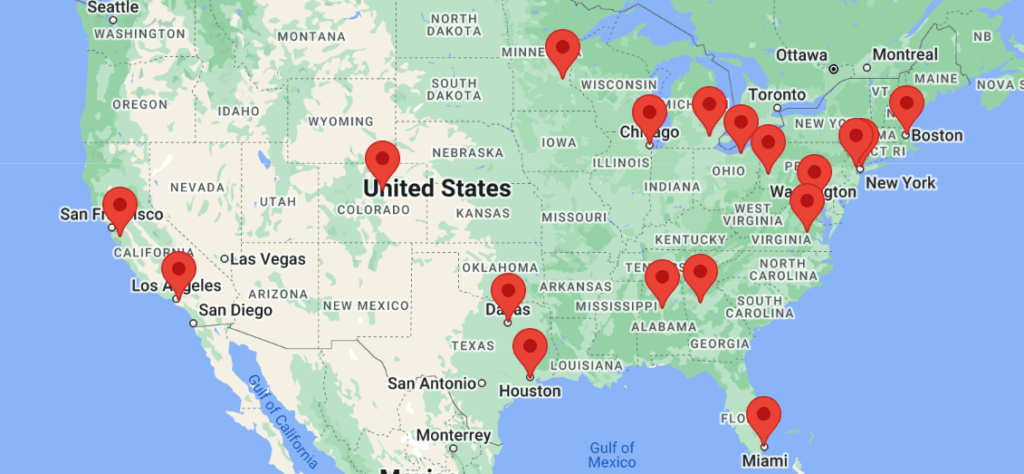
Access to specialists (respirology, physiatry) may be limited, particularly if you do not live in or near a major city.
If you or your patients with SCI are not already connected, please try to gain access to a physiatrist near you. Refer to the list of SCI centers worldwide below:
- Australia (Queensland Spinal Cord Injuries Service): https://www.health.qld.gov.au/qscis
- Canada: https://praxisinstitute.org/research-care/key-initiatives/national-sci-registry/registry-sites
- Europe (enrolled in European Multicenter Spinal Cord Injury Study): https://www.emsci.org/index.php/members
- UK: https://www.brainandspine.org.uk/wp-content/uploads/2018/03/BSF_List-of-Neurocentres-in-the-UK.pdf
- USA: https://www.spinalcord.com/spinal-cord-injury-hospitals-rehabilitation-directory
(Please email SCIRE Professional if we do not have a list for your country)
- Berlly M, Shem K. Respiratory management during the first five days after spinal cord injury. J Spinal Cord Med, 2007;30(4):309-318.
- Galeiras Vázquez R, Rascado Sedes P, Mourelo Fariña M, Montoto Marqués A, Ferreiro Velasco ME. Respiratory management in the patient with spinal cord injury. Biomed Res Int, 2013;2013.
- Garshick E, Kelley A, Cohen SA, et al. A prospective assessment of mortality in chronic spinal cord injury. Spinal Cord. 2005;43(7):408-416. doi:10.1038/sj.sc.3101729
- Model Systems Knowledge Translation Center (MSKTC). Respiratory Health and Spinal Cord Injury. Published August, 2015. Accessed on June 10, 2024.
- Reyes MRL, Elmo MJ, Menachem B, Granda SM. A primary care provider’s guide to managing respiratory health in subacute and chronic spinal cord injury. Top Spinal Cord Inj Rehabil. 2020;26(2):116-122. Doi:10.46292/sci2602-116
- Warren PM, Awad BI, Alilain WJ. Reprint of “Drawing breath without the command of effectors: the control of respiration following spinal cord injury”. Respir Physiol Neurobiol, 2014;204:120-130.
- https://www.healthline.com/health/bronchitis-vs-pneumonia
- Respiratory Infections After SCI. Published on December 3, 2020. Available at: https://www.spinalcord.com/respiratory-infections-after-a-spinal-cord-injury
For Clinical Practice Guideline recommendations based on your patient’s level of injury and specific complaint, click here for the Can-SCIP Coach App.
For more information see our Respiratory Management (Rehab) Module.
Disclaimer
All content and information on this website is for informational and educational purposes only, does not constitute medical advice, and does not establish any kind of patient-client relationship by your use of this website. The information here has been curated by experts in spinal cord injury treatment but it is not a substitute for actual medical consultation. Always see a medical professional directly for specific treatment for your particular needs including any professional, health-related, legal, medical, or financial decisions.