Experimental Studies
Epidural spinal cord stimulation (SCS) was originally investigated by researchers looking to recover voluntary motor function in case-studies of people with SCI (e.g., Harkema et al. 2011). Based on positive results in voluntary neural function other than motor below the level of injury, researchers have reasoned that bladder, bowel, and sexual dysfunction would be most logical to study in parallel (Pettigrew et al. 2017). Implanted epidural spinal cord stimulation is performed in some countries, but still does not have federal approval in most countries (US, Canada, UK, etc.).
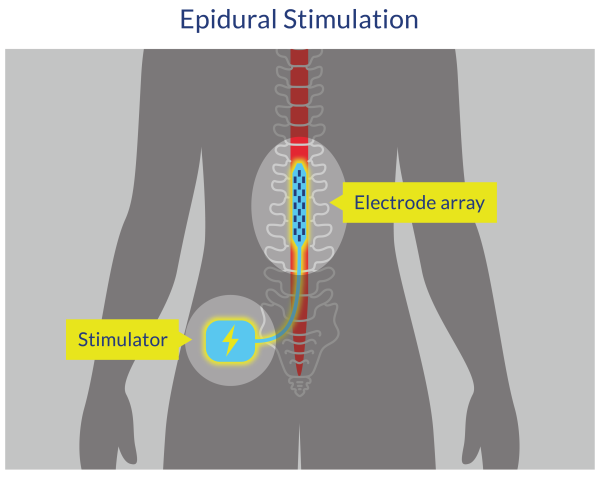
Figure 2. Epidural Spinal Cord Stimulation
Other experimental treatments for neurogenic bowel after SCI include type A-botulinum toxin (BTX-A), Wharton jelly mesenchymal stromal cell intrathecal infusion, and osteopathic manipulative treatment.
Discussion
There are several innovations that have been developed to treat people with SCI, but they are still considered ‘experimental’ as there is little to no evidence supporting their use, their safety and efficacy have not yet been fully established, and/or they have not yet been approved for widespread use.
For example, epidural spinal cord stimulation (eSCS) is currently being investigated to restore volitional movement and autonomic function in people with SCI. Darrow et al. (2019) presented findings from the Epidural Stimulation After Neurologic Damage clinical trial (E-STAND). One objective was to determine whether eSCS could restore autonomic control of bowel function. Both participants who received the implantation had no bowel function improvements observed with the epidural SCS, and participant 2 had a worsening of NBD severity. However, participant 2 did report that time required for bowel care decreased from 90 minutes to less than 30 minutes. Further studies are required to confirm changes in bowel function and management with epidural spinal cord stimulation.
Botox (BTX-A) infiltration of the external anal sphincter resulted in significant constipation symptom improvements in one clinical trial (p=0.02; Valles et al. 2021). Another clinical trial investigating Wharton jelly cell intrathecal infusion at the L3-4 intervertebral level found no significant changes in constipation, fecal incontinence, or anorectal manometry parameters (Albu et al. 2021).
DiMarco et al. (2021) investigated an experimental, airway suppression secretion management using electrical stimulation. Electrodes were inserted on the upper lumbar, dorsal surface of the spinal cord and the intervention resulted in increased airway pressure generation as well as reduced bowel management time (mean BM 118 ± 34 min to 18 ± 2 min at week 21 (p<0.05) (DiMarco et al. 2021).
Conclusion
There is level 1 evidence from a pilot RCT (Valles et al. 2021) that type A-botulinum toxin infiltration in the external anal sphincter improved constipation symptoms (p=0.02) by decreasing anal canal pressure and EAS contraction. Fecal incontinence, colonic transit time, and quality of life did not significantly change after the intervention.
There is level 1 evidence from one double blinded RCT (Tamburella et al. 2022) that osteopathic manipulative treatment which had focus on the abdominal region may have a positive effect on neurogenic bowel function symptoms and perceptions in comparison to a manual placebo treatment for people with SCI and NBD.
There is level 1 evidence from a randomized controlled trial (Albu et al. 2021) that while wharton jelly mesenchymal stromal cell intrathecal infusion demonstrated a positive effect on sensory perception below level of injury compared to a placebo infusion, the treatment did not significantly improve bowel function in people with complete, thoracic SCI.
There is level 2 evidence (DiMarco et al. 2021) that using spinal cord stimulation to activate muscles that induce a cough improves bowel management time and quality of life for select individuals with cervical SCI.
