Neurological and Functional Status
Several studies have identified patterns of neurological and/or functional improvement over the first few months post-injury. Most of these studies examine neurological and/or functional status and associated changes between rehabilitation admission and discharge. Table 4 summarizes various reports in the literature for neurological and/or functional status organized by jurisdiction and by the time period for which the data was collected. Data were only included if the underlying sample was deemed representative of an overall heterogeneous population of individuals with SCI (i.e., unselected sample of a single or multi-centre study).
Discussion
The AIS represents an internationally recognized system for the classification of individuals with SCI, and as such, has been employed to characterize overall improvement in the neurological status of people with SCI (ASIA 2002). It is somewhat similar to earlier systems such as the Frankel grading classification system. The AIS is an ordinal 5 grade scale classifying individuals from “A” to “E” with “A” designating those with complete SCI and “E” designating individuals with normal sensory and motor function. Most notably, DeVivo (2007), Pagliacci et al. (2003), Celani et al. (2001), Marino et al. (1999) and DeVivo et al. (1991) employed large multi-centre databases and found that individuals with incomplete injuries (especially AIS B or C) were more likely to improve at least 1 grade over the course of rehabilitation. In particular, DeVivo et al. (1991) reported that 45.2% and 55.9% of those initially admitted as AIS B and C respectively improved at least 1 AIS grade as compared to only 10.3% and 7.3% of individuals initially classified as AIS A or D respectively. Over the period of 1973-2006, DeVivo (2007) reported that there was an 8.8% increase in likelihood that those classified as AIS A at admission would improve to AIS B at discharge. Other reports have presented similar findings and data culled from a sample of these investigations have been summarized in Figure 1. Figure 1 illustrates the proportion of persons assessed at each AIS (or Frankel) grade status (i.e., A, B, C or D) at discharge from rehabilitation relative to the proportion of people at each AIS level at rehabilitation admission for each of the studies (Burke et al. 1985; Catz et al. 2002; M. DeVivo 2007; Marino et al. 1999; Pagliacci et al. 2003; Sumida et al. 2001). This provides an indication of the degree of neurological recovery that occurs over the period of rehabilitation. It should be noted that for each study (i.e., jurisdiction) the admission and discharge time points are variable relative to the time of injury although these all are typically within the first six months following injury. In addition, all datasets consisted of relatively unselected patients with traumatic SCI, other than the report by Sumida et al. (Sumida et al. 2001) which included patients with SCI of both traumatic and non-traumatic etiology.
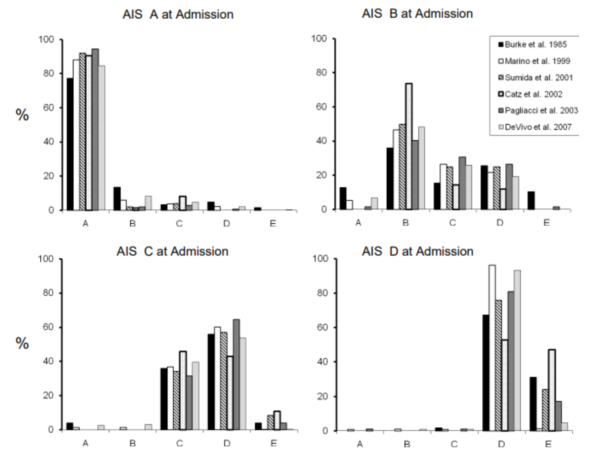
Figure 1. Discharge or Frankel Grades for each initial admission AIS grade
As one can see, it is striking how similar these patterns of AIS conversion rates are across health systems (i.e., Australia, Israel, Italy, Japan, United States) with only Catz et al. (2002) (i.e., Israel) providing somewhat disparate results. Overall, AIS A patients comprise from 40-50% of individuals admitted to SCI rehabilitation centres and a similar, but slightly reduced percentage of those are assessed AIS A at discharge. AIS B and AIS C patients comprise ~5-15% and ~10-30% respectively with moderate reductions in these percentages manifest at discharge. Conversely, those assessed AIS D comprise ~15-25% of those admitted which increases to ~25-35% by discharge.
The majority of patients assessed AIS A at admission remain so at discharge, whereas a much greater proportion of individuals assessed AIS B recovered significant motor function during rehabilitation so as to be assessed AIS C or D. The conversion rate is even greater for those assessed initially as AIS C but much less so for those assessed as AIS D.
These conversion rates appear similar across these studies and therefore provide a base for comparison with other findings. For example, Moslavac et al. (Moslavac et al. 2008) reported data for a centre-based study in Croatia at which all national cases of SCI resulting from road traffic accidents received rehabilitative care. In this case, although 49% of people were AIS A at admission and 93% of these remained AIS A at discharge, there was a tendency for greater proportions of persons making conversions to AIS D or E of those assessed with an incomplete injury at admission. Importantly, Wilde et al. (2020) found that interhospital transfer does not reduce functional recovery.
Similarly, many individuals also make significant functional gains during comprehensive inpatient rehabilitation. Most often, functional status has been assessed at admission and discharge from rehabilitation using the FIM (De Vivo et al. 1991; Muslumanoglu et al. 1997; Tooth et al. 2003; Chan & Chan 2005) or MBI (Yarkony et al. 1987). Typically, functional gains are greater with rehabilitation for those with incomplete injuries as compared to complete injuries and for those with paraplegia as compared to those with tetraplegia (Chan & Chan 2005; De Vivo et al. 1991; Muslumanoglu et al. 1997; Tooth et al. 2003). In particular, DeVivo et al. (1991) reported similar average FIM gains for those with incomplete and complete paraplegia and incomplete tetraplegia (i.e., 37, 36 and 34 respectively) but much reduced gains for those with complete tetraplegia (i.e., 15). For the most part increases seen in the FIM have been attributed to motor FIM changes with little change in cognitive FIM scores at least partly due to an apparent ceiling effect (Chan & Chan 2005).
Conclusions
There is level 4 evidence that a significant proportion of people (~50%) initially assessed as AIS B and C will improve by at least one AIS grade in the first few months post-injury concomitant with inpatient rehabilitation. Fewer individuals (~10%) initially assessed as AIS A and D will improve by one AIS grade.
There is level 4 evidence that individuals make significant functional gains during inpatient rehabilitation, more so for those with complete and incomplete paraplegia and incomplete tetraplegia.
