Spinal Cord Stimulation on OH
Spinal cord stimulation, or epidural stimulation, is an emerging intervention for managing OH in individuals with SCI. By delivering electrical currents to spinal networks below the level of injury, these techniques may help modulate cardiovascular responses during postural changes and reduce symptoms of orthostatic intolerance by stimulating the nerves to cause muscle contractions. An electrode is implanted into the epidural space behind the spine and electrical currents are sent directly to the bypassing brain-to-spinal cord pathways to help reactivate remaining intact neural networks that facilitate the movements to stand and walk.
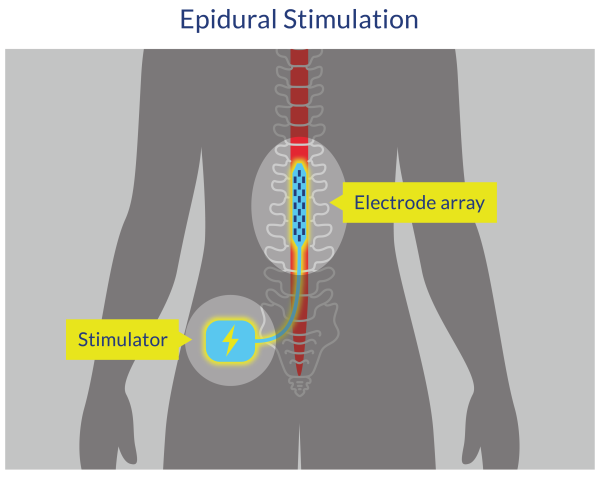
Figure 3. Epidural Spinal Cord Stimulation
Transcutaneous spinal stimulation (TSS) is another type of spinal cord stimulation that is non-invasive and uses electrical impulses applied to the skin to stimulate the spinal cord and potentially restore or improve motor function.
Discussion
A few studies have examined the effect of scES on OH symptoms and challenges. Preliminary results show that scES upon standing may increase sBP, dBP, and HR in individuals who demonstrate orthostatic intolerance (Aslan et al. 2018; Harkema et al. 2018b), but does not affect those who do not experience OH symptoms (Aslan et al. 2018). While the cessation of scES results in BP and HR returning to baseline (Harkema et al. 2018b), Harkema et al. (2018a) suggested that daily scES training may provide individuals with a BP increase and HR decrease upon sitting even when presented with orthostatic stress without stimulation.
Moreover, Aslan et al. (2018) found that individuals who demonstrated orthostatic intolerance upon standing experienced dizziness or fatigue without scES; however, these symptoms were mitigated with the use of scES. Further, individuals reported enhanced (1) feelings of alertness or heightened awareness; (2) ability to project their voice and have conversations; (3) capacity to breathe and cough; and (4) overall sense of well-being with scES (Harkema et al. 2018b).
Similarly, transcutaneous stimulation is a promising non-invasive tool for treatment of OH in people with SCI. A study by Phillips et al. (2018) found that transcutaneous stimulation at the TVII level reduced OH in all participants. However, heart rate did not decrease with stimulation, resulting in SV still being reduced. Additionally lower-limb skeletal muscle contraction did not occur, meaning that the pressor response was not attributed to skeletal muscle pump action.
Further research will be necessary to expand on the possibilities of spinal stimulation therapy and its effects on OH and other associated conditions in people with SCI.
Conclusion
There is level 4 evidence (from one pre-post) (Aslan et al. 2018) that scES reduced the drop in BP and orthostatic symptoms upon standing in individuals with SCI who demonstrated orthostatic intolerance.
There is level 2 evidence (from one prospective cohort study) (Harkema et al. 2018a) that daily CV-scES training reduced the drop in BP from supine to sitting, even when presented with orthostatic stress without stimulation,
There is level 2 evidence (from one prospective cohort study) (Harkema et al. 2018b) that CV-scES increases BP and enhanced individuals’ (1) feelings of alertness or heightened awareness; (2) ability to project their voice and have conversations; (3) capacity to breathe and cough; and (4) overall improved sense of well-being.
There is level 4 evidence (from one pre-post) (Phillips et al. 2018) that TSS at the TVII level reduced OH in all participants; however, the reduction in blood pressure following TSS cannot be attributed to skeletal muscle pump action.
