Introduction
Blood pressure instability, including orthostatic hypotension (OH), is common in people with spinal cord injuries (SCI). OH is defined by The Consensus Committee of the American Autonomic Society and the American Academy of Neurology (CCAAS & AAN 1996) as a decrease in systolic blood pressure of at least 20mmHg, or a reduction in diastolic blood pressure of at least 10mmHg occurring within 3 minutes upon the assumption of an upright position from supine (i.e., laying down), regardless of the presence of symptoms (Krassioukov et al. 2012). OH occurs during the acute period of SCI and persists in many individuals for several years (Sidorov et al. 2008; Claydon et al. 2006; Frisbie & Steele 1997).
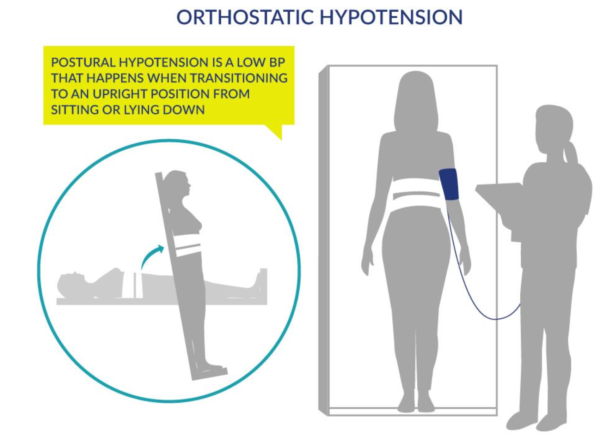
Figure 1. Orthostatic Hypotension as generated by Postural Changes
Normally, the nervous system automatically constricts or dilates the blood vessels to balance blood pressure during postural changes; however, this ability may be compromised after an SCI, particularly for people with injuries at or above T6, resulting in OH. During an episode of OH, symptoms including dizziness, blurred vision, and fainting, may or may not occur.
Table 1. Signs and Symptoms of OH
- Light-headedness
- Dizziness
- Blurred vision
- Fatigue
- Muscle weakness
- Fainting
Studies have shown that delayed BP recovery and OH are associated with future risk of falls, fractures, fainting, stroke, cardiovascular disease, and even earlier death (10-year mortality rate of 50-64%). Further, standard mobilization treatment during physiotherapy (e.g., sitting or standing) is reported to trigger BP decreases that are diagnostic of OH in 74% of people with SCI and cause symptoms in 59% (Illman et al. 2000). Therefore, simple activities like sitting up or eating may trigger BP drops and cause symptoms of OH, discouraging people with SCI from participating in rehabilitation, exercise, or completing activities of daily living; thus creating the need for other management methods.
Cite this chapter: Krassioukov A, Sun E, Wecht JM, Teasell RW, Eng JJ (2025). Orthostatic Hypotension Following Spinal Cord Injury. In Eng JJ, Teasell RW, Miller WC, Townson AF, Hsieh JTC, Noonan VK, Mortenson WB, Loh E, Bateman EA, Allison D, Unger J, Joyce S, Querée M, editors. Spinal Cord Injury Rehabilitation Evidence. Vancouver: p 1- 64. Available at: https://scireproject.com/evidence/orthostatic-hypotension/introduction/
