Measurement Property Summary
Number of studies reporting psychometric properties: 4
Interpretability
- MCID: not established in SCI population
- SEM: not established in SCI population
- MDC: not established in SCI population
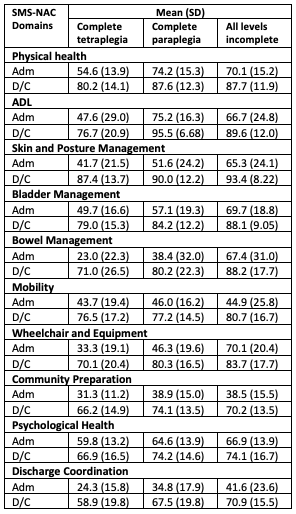
- Typical values: Mean (SD) scores for each SMS-NAC domain:
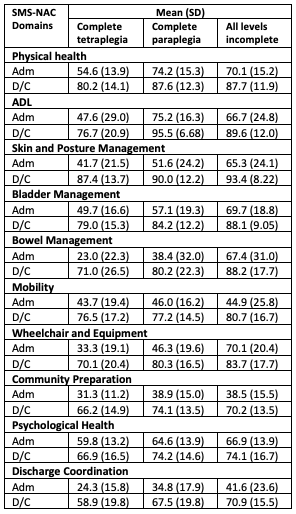
Admission (adm), discharge (D/C)
(Eaton et al. 2022; n=191; 139 males, 56 females; mean (SD) age: 53.0 (17.5) years; 51 tetraplegia complete (C1-C8 A/B/C), 77 paraplegia complete (T1-L5 A/B/C), 67 incomplete (C1-L5 D); mean (SD) time from injury to rehabilitation: 412.6 (2895.7) days)
Reliability – Moderate to High
Number of studies reporting reliability data: 3
- Moderate to High test-retest reliability:
- Overall α = 0.8238
- Subscale α = 0.694-0.904
(Berry & Kennedy 2002; n=43; 38 males, 5 females; mean (SD) age: 42.2 (14.6) years; complete and incomplete tetraplegia and paraplegia)
- Moderate to High internal consistency:
- Overall α = 0.83
- Subscale α = 0.6729-0.9467
(Kennedy et al. 2003; n=192; 147 males; 45 females; mean (SD) age: 40.7 (16.5) years, tetraplegia and incomplete SCI)
-
- Overall α = 0.889
- All subscales α = > 0.7
(Kennedy et al. 2012; n=193; 143 males, 50 females; mean age: 46.6 years; tetraplegia and paraplegia; complete and incomplete injuries)
Validity – Moderate to High
Number of studies reporting validity data: 1
- High correlation between the NAC ADL with SCIM-II (r = 0.873), the NAC Bladder & Bowel with SCIM-II (r = 0.754), and the NAC Mobility with SCIM-II (r = 0.696)
- High correlation between the NAC psychological issues (mood subsection) with HADS (r = -0.726).
- Moderate to High correlation between the NAC psychological issues (full subscale) with HADS (r = -0.523).
(Berry & Kennedy 2002; n=43; 38 males, 5 females; mean (SD) age: 42.2 (14.6) years; complete and incomplete tetraplegia and paraplegia)
Responsiveness
- Responsiveness to change:
- There was an average increase of 60% across all domains of the SMS-NAC (all domains except psychological health demonstrated an increase of more than 20%).
- Weak to moderate differences between rehabilitation scores obtained based on injury level: In nine domains of the SMS-NAC, excluding mobility, there was a significant main effect of level of injury, though the effect sizes ranged from weak (partial η2 = 0.05 for SMS-NAC psychological health, the smallest effect size) to moderate (partial η2 = 0.30 for SMS-NAC activities of daily living, the largest effect size).
(Eaton et al. 2022; n=191; 139 males, 56 females; mean (SD) age: 53.0 (17.5) years; 51 tetraplegia complete (C1-C8 A/B/C), 77 paraplegia complete (T1-L5 A/B/C), 67 incomplete (C1-L5 D); mean (SD) time from injury to rehabilitation: 412.6 (2895.7) days)
Floor/Ceiling Effect
No values were reported for the presence of floor/ceiling effects in the NAC for the SCI population.
Reviewers
Dr. Carlos L. Cano-Herrera, Tyra Chu
Date Last Updated
December 31, 2024